Increased Infection Risks After COVID-19 Infections
Waves of COVID-19 infections have continued all around the world as new variants appear. The expectation that previous infections would reduce the probability or severity of the disease has proved to be incorrect [1].
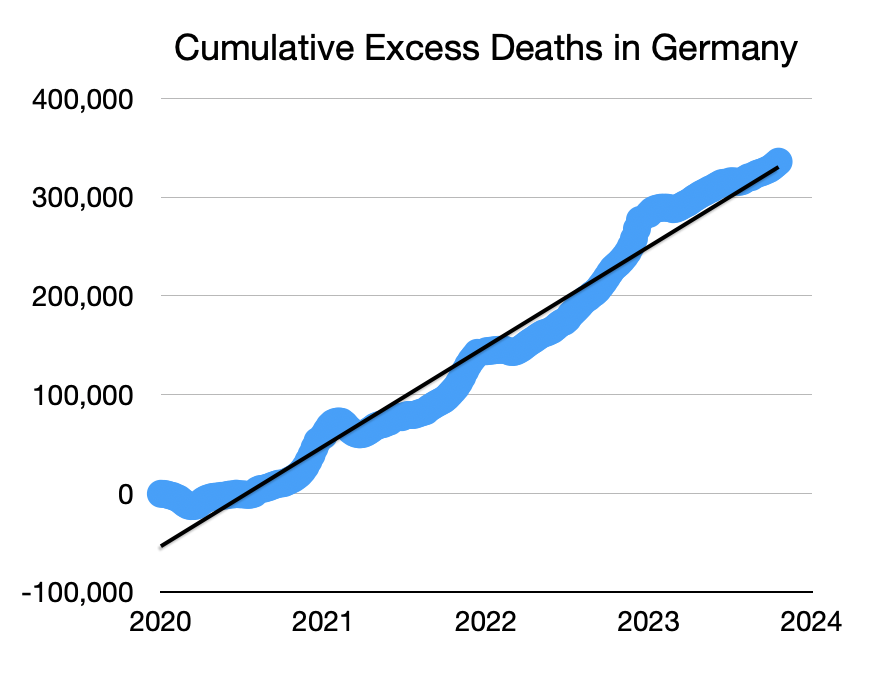
While deaths during the acute phase have been decreasing, in part due to improved disease treatment and vaccination, excess mortality continues to be high [2] (See Figures 1 and 2) and evidence shows that repeated infections deteriorate health and increase many health risks [3,4], including long COVID, autoimmune disease [5], stillbirths [6], other infections, including RSV [7], and many more [8].

Some of these adverse effects have been related to a deterioration of the immune system after a SARS-CoV-2 infection [9,10]. The probability of Long COVID and adverse health impacts increases with repeated infections.[11]
Two articles mentioned below (among many more) show that significantly higher risk from other infections occurs for those who have suffered from COVID, consistent with many studies showing that the immune system deteriorates due to the infection.[12]
The first article [7] evaluated the risk of RSV infections in children. It found that comparing children aged 0-5 with or without a COVID infection and otherwise similar to each other, the occurrence of a RSV infection was 40% higher for those that had a COVID infection. The same results were obtained when looking at two separate years.
The second article [8], from 2021 clearly demonstrates the increased occurrence of various types of infections in adults, as highlighted in Table 1. It is concerning that respiratory, sinus, skin, urinary tract, or intestinal infections were between 1.24 and 1.5 times higher, while bacterial, fungal, and parasitic infections were 1.2 to 1.8 times higher. However, what is truly alarming is the increased rates of viral infections at 4.4 times higher, along with higher rates of STDs (excluding HIV and hepatitis), influenza and pneumonia more generally. An indication of the overall impacts of infections can be seen in nearly a 15-fold increase in reports of follow on effects of infectious disease conditions.
This spiral of infections and their consequences is not sustainable. The health of the population will keep on deteriorating. We have measures to reduce the impact of COVID-19 [5], why not use them?
| Type of Infection | Multiplier after covid infection |
|---|---|
| RSV infection in children 0-5 [7] | 1.40X |
| Other respiratory infections [8] | 1.40X |
| Bacterial infections [8] | 1.43X |
| Fungal infections [8] | 1.21X |
| Parasitic infections [8] | 1.82X |
| Viral infections [8] | 4.4X |
| Sinusitis [8] | 1.21X |
| Skin infections [8] | 1.24X |
| Urinary tract infections (UTI) [8] | 1.37X |
| Intestinal infections [8] | 1.50X |
| STDs (excluding HIV, hepatitis) [8] | 1.39X |
| Acute bronchitis [8] | 1.34X |
| Acute and chronic tonsillitis [8] | 1.62X |
| Influenza [8] | 2.9X |
| Pneumonia (except that caused by tuberculosis) [8] | 3.28X |
| Sequelae of infectious disease conditions [8] | 14.6X |
Table 1: The increase in incidence after a COVID infection compared to the incidence for matched individuals without a COVID infection [7,8].
References
- Kuang, S., Earl, S., Clarke J., Zakaria, D., Demers, A, Aziz, S., Experiences of Canadians with long-term symptoms following COVID-19, Insights on Canadian Society. December. Statistics Canada Catalogue no. 75-006-X. https://www150.statcan.gc.ca/n1/pub/75-006-x/2023001/article/00015-eng.htm
- Mortality, by week: Excess deaths by week, 2020-2023 https://stats.oecd.org/index.aspx?queryid=104676
- DeVries, A., Shambhu, S., Sloop, S., & Overhage, J. M. (2023, March), One-Year Adverse Outcomes Among US Adults With Post–COVID-19 Condition vs Those Without COVID-19 in a Large Commercial Insurance Database, JAMA Health Forum. 2023;4(3):e230010. https://doi.org/10.1001/jamahealthforum.2023.0010
- Sharma, C., Bayry, J. High risk of autoimmune diseases after COVID-19. Nat Rev Rheumatol 19, 399–400 (2023). https://doi.org/10.1038/s41584-023-00964-y
- Špela Šalamon Andrew Ewing Greta Fox Stephane Bilodeau Carlos Gershenson Matti TJ Heino Yaneer Bar-Yam SARS-CoV-2 and COVID-19: From Crisis to Solution. WHN Science Communications 2024; 5 (1): 1-1. https://doi.org/10.59454/whn-2401-334
- Magnus, M. C., Örtqvist, A. K., Urhoj, S. K., Aabakke, A., Mortensen, L. H., Gjessing, H., … & Håberg, S. E. (2023). Infection with SARS-CoV-2 during pregnancy and risk of stillbirth: a Scandinavian registry study. BMJ Public Health, 1(1). https://doi.org/10.1136/bmjph-2023-000314
- Wang L, Davis PB, Berger N, et al Association of COVID-19 with respiratory syncytial virus (RSV) infections in children aged 0–5 years in the USA in 2022: a multicentre retrospective cohort study Family Medicine and Community Health 2023;11:e002456. http://doi.org/10.1136/fmch-2023-002456
- Supplementary Table 2 in Al-Aly, Z., Xie, Y. & Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 594, 259–264 (2021). https://doi.org/10.1038/s41586-021-03553-9
- Phetsouphanh, C., Darley, D.R., Wilson, D.B. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol 23, 210–216 (2022). https://doi.org/10.1038/s41590-021-01113-x
- Chattopadhyay P, Khare K, Kumar M, Mishra P, Anand A, Maurya R, Gupta R, Sahni S, Gupta A, Wadhwa S, Yadav A, Devi P, Tardalkar K, Joshi M, Sethi T and Pandey R (2022) Single-cell multiomics revealed the dynamics of antigen presentation, immune response and T cell activation in the COVID-19 positive and recovered individuals. Front. Immunol. 13:1034159. http://doi.org/10.3389/fimmu.2022.1034159
- Bowe, B., Xie, Y. & Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med 28, 2398–2405 (2022). https://doi.org/10.1038/s41591-022-02051-3
- Ewing, A., COVID-19 and Immune Dysregulation, a Summary and Resource. WHN Science Communications 2023; 4 (3): 1-1. https://doi.org/10.59454/whn-2303-765
- Destatis, Population, Deaths, Life Expectancy https://www.destatis.de/EN/Themes/Society-Environment/Population/Deaths-Life-Expectancy/_node.html


