After a COVID infection, people may experience ongoing or new symptoms due to the damage that the virus has done to the body. This occurs even in those who have mild or asymptomatic infections and in young and healthy individuals. The damage affects the heart, brain, kidney, immune system, and other organs.
How many people are affected?
Early estimates varied widely, especially since early studies often looked at only a few of the many long COVID symptoms. However, recent large meta-analyses and systematic reviews report similar prevalence figures of around 1 in 3 of those with registered COVID-19 overall, and around 50% of those hospitalized [1-6]. Since many symptomatic studies don’t include a control group, estimates based upon symptoms are still somewhat uncertain (See note). This uncertainty generally doesn’t apply to organ damage studies where many show higher than 50% prevalence [7-9]. For example, impacts on cognitive function (IQ) happen even for those who have mild disease and do not report that they have long COVID symptoms [10].
Do children get long COVID?
Yes, many studies report that children have about a 10-20% rate of long COVID symptoms. Notably, a review of 21 studies, corresponding to more than 80,000 children and adolescents, show that the prevalence of long COVID is 25% [11,12]. While the general conclusions are converging—i.e., children can experience the wide range of debilitating symptoms that are found in adults—the exact nature of the studies’ results depend on which symptoms are measured.
What are the symptoms?
There are many symptoms, the most common of which include severe tiredness, shortness of breath, worsening of symptoms after activities, memory problems, “brain fog,” heart palpitations, chest pain, headaches, mood and sleep disturbances, muscle weakness, and loss or change of smell and taste [13]. Blood clotting is a common problem [14].
What are the consequences?
There is a wide range of severity, with some having mild symptoms, while others are unable to continue regular activities such as walking or climbing stairs, or returning to their previous work. Normal life is often disrupted.
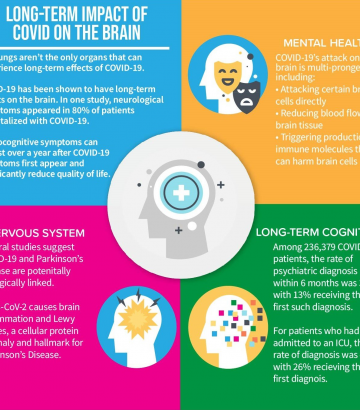
What does the organ damage lead to?
The organ damage can lead to strokes, heart attacks or heart failure [15], pulmonary embolism, kidney failure, or liver injury, to mention some. In a predominantly older, male population, the risk of cardiovascular events (not including other organ damage) in the first year was found to be about 4%, 3% in those with mild cases, 16% in those who were hospitalized, and 31% in those who were in ICUs [15, Suppl. Table 8]. The immune system itself is harmed, affecting multiple cell types and impairing immune function over time [16] as well as causing signs of several different auto-immune diseases [17]. This dramatically increases the impact of COVID on those who were infected. Excess burden of death from all causes in the first 6 months after the acute phase of a COVID infection have been reported to be 2.0% in non-vaccinated and 1.3% in those vaccinated (breakthrough cases) [18].
How is it related to other chronic diseases?
Connections have been found to the biology of autoimmune diseases, multiple sclerosis [17,19], Alzheimer’s [20], Parkinson’s [21], and harmful effects similar to the impacts of chemotherapy for cancer [22].
How long does it last?
Symptoms often last for months and there are many people who have had long COVID symptoms since the beginning of the pandemic 2 years ago. For many, the symptoms improve over time, but for others they can come and go, and for some they even get worse. Among patients with symptoms 2 months after the acute illness, 85% still reported symptoms after one year [23]. Experience with SARS1, the most closely related disease, indicates debilitating symptoms can last for many years [24].
What causes long COVID?
The virus that causes COVID enters cells that have a certain receptor (ACE2) and often damages those cells. The cells around blood vessels have many such receptors. In many ways, COVID is a vascular disease more than a respiratory (lung) disease (we think about it as a lung disease because it often starts there). The virus can also enter other cells in different organs and cause damage, as can the process of inflammation itself.
What have scientists learned about the mechanisms of long COVID?
Researchers are identifying the multiple specific ways that long COVID symptoms and organ damage arise. These include: persistent viral replication, direct organ damage, auto-immune disease, reactivation of “zombie” virus fragments from ancestral infections with other viruses [25,26], and others. For example, the virus (SARS-CoV-2) has been found in the gut in patients with long COVID symptoms 10 months after the acute illness [27].
Do vaccines prevent long COVID?
Vaccines may provide some but limited prevention. While some studies have found that vaccination reduces the risk of getting long COVID after breakthrough infections by about 50% [28,29], a new, large study found only 15% protection [18], and others find that it has little effect on many consequences of the disease [30].
Is it possible to have long COVID without realizing it?
Since long COVID may start after an initial recovery from acute COVID-19, which may be asymptomatic, and testing is scarce in many regions, people may suffer from long COVID without being aware of the link to a previous COVID-19 infection.
What can we do about long COVID?
Our actions can make a great difference, helping individuals recognize when their symptoms may be due to long COVID, recognizing and supporting those who have long COVID—enabling them to support themselves through work flexibility and supporting them in other daily activities, supporting the study of potential approaches to prevention and treatments, and preventing infections and reinfections in ourselves and others that lead to more cases of long COVID.
REFERENCES
- Chen et al: Global Prevalence of Post-Acute Sequelae of COVID-19 (PASC) or Long COVID: A Meta-Analysis and Systematic Review. Journal of Infectious Diseases, 2022. https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiac136/6569364
- Groff et al: Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection. A Systematic Review. Jama Network Open, 2021. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784918
- Sørensen et al: A nationwide questionnaire study of post-acute symptoms and health problems after SARS-CoV-2 infection in Denmark. Nature Communications, 2022. https://www.nature.com/articles/s41467-022-31897-x.
- Yoo et al: Factors Associated with Post-Acute Sequelae of SARS-CoV-2 (PASC) After Diagnosis of Symptomatic COVID-19 in the Inpatient and Outpatient Setting in a Diverse Cohort. J of Gen Int Med, 2022. https://link.springer.com/article/10.1007/s11606-022-07523-3#article-info
- Sugiyama et al: Long COVID occurrence in COVID-19 survivors. Nature Scientific Reports, 2022. https://www.nature.com/articles/s41598-022-10051-z
- Seessle et al: Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin Inf Diseases, 2022. https://academic.oup.com/cid/article/74/7/1191/6315216
- Dennis et al: Multi-organ impairment and Long COVID: a 1-year prospective, longitudinal cohort study. Pre-print. MedRxiv, 2022. https://www.medrxiv.org/content/10.1101/2022.03.18.22272607v1
- Puntmann et al: Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiology, 2021. https://jamanetwork.com/journals/jamacardiology/fullarticle/2768916
- Petersen et al: Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur Heart Journal, 2022. https://academic.oup.com/eurheartj/article/43/11/1124/6499078
- Hampshire et al: Cognitive deficits in people who have recovered from Covid-19. Lancet eClin Med 2021. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00324-2/fulltext
- Lopez-Leon et al: Long COVID in Children and Adolescents: A Systematic Review and Meta-analyses. Nature Scientific Reports, 2022. https://www.nature.com/articles/s41598-022-13495-5
- Hamzelou, J: A battle is raging over long covid in children. MIT Technology Review, 2022. https://www.technologyreview.com/2022/04/06/1048984/battle-over-long-covid-children/
- Alkodaymi et al: Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol and Infection, 2022. https://www.sciencedirect.com/science/article/pii/S1198743X22000386
- Burn et al: Venous or arterial thrombosis and deaths among COVID-19 cases: a European network cohort study. Lancet Infectious Diseases, 2022. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00223-7/fulltext
- Xie et al: Long-term cardiovascular outcomes of COVID-19. Nature, 2022. https://www.nature.com/articles/s41591-022-01689-3
- Phetsouphanh et al: Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nature, 2022. https://www.nature.com/articles/s41590-021-01113-x
- Su et al: Multiple early factors anticipate post-acute COVID-19 sequelae. Cell, 2022. https://www.cell.com/cell/fulltext/S0092-8674(22)00072-1
- Al-Aly et al: Long COVID after breakthrough SARS-CoV-2 infection. Nature Med 2022. https://www.nature.com/articles/s41591-022-01840-0
- Bellucci et al: Multiple Sclerosis and SARS-CoV-2: Has the Interplay Started? Frontiers In Immunology, 2021. https://www.frontiersin.org/articles/10.3389/fimmu.2021.755333/full#B32
- Schwabenland et al: Deep spatial profiling of human COVID-19 brains reveals neuroinflammation with distinct microanatomical microglia-T-cell interactions. Immunity, 2021. https://www.cell.com/immunity/fulltext/S1074-7613(21)00246-6
- Shen et al: SARS-CoV-2 invades cognitive centers of the brain and induces Alzheimer’s-like neuropathology. bioRxiv, 2022. https://www.biorxiv.org/content/10.1101/2022.01.31.478476v2
- Hamoy et al: Parkinson’s disease secondary to COVID-19: a systematic review. Research, Society and Development, 2021. https://rsdjournal.org/index.php/rsd/article/view/24397
- Fernández-Castañeda et al: Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Cell, 2022. https://www.sciencedirect.com/science/article/pii/S0092867422007139
- Chai, Politi, SARS 10 years later: How are survivors faring now?, Global News, https://globalnews.ca/news/404562/sars-10-years-later-how-are-survivors-faring-now/
- Tran et al: Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nature Communications, 2022. https://www.nature.com/articles/s41467-022-29513-z
- Charvet et al: SARS-CoV-2 induces human endogenous retrovirus type W envelope protein expression in blood lymphocytes and in tissues of COVID-19 patients. MedRxiv, 2022. https://www.medrxiv.org/content/10.1101/2022.01.18.21266111v2
- Natarjan et al: Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med, 2022. https://www.cell.com/med/fulltext/S2666-6340(22)00167-2
- Reardon: Long COVID risk falls only slightly after vaccination, huge study shows Nature, 2022. https://www.nature.com/articles/d41586-022-01453-0
- Venkatesan: Do vaccines protect from Long Covid? Lancet Respiratory Medicine, 2022. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(22)00020-0/fulltext
- Taquet et al: Six-month sequelae of post-vaccination SARS-CoV-2 infection: A retrospective cohort study of 10,024 breakthrough infections. Brain, Behavior, and Immunity, 2022. https://www.sciencedirect.com/science/article/pii/S0889159122001118
Some methodological issues regarding prevalence studies on long COVID
The lack of control groups have been a limitation to many of the current studies on the prevalence of long COVID. However, there is an increasing challenge in including control groups, in that many people have been infected with SARS-CoV-2 without being registered as such, sometimes even without knowing it themselves. If many in the control groups have indeed been infected with SARS-CoV-2, the differences between the control group and those we know have been infected, will be smaller than it otherwise would have been. For instance, one recent study on symptoms did use a control group but did not use serological studies to determine infections in the control group. Instead: “Participants’ COVID-19 positivity was defined as either a positive SARS-CoV-2 test or a physician’s diagnosis of COVID-19, which was based on the evolving clinical case definition issued by the Dutch Institute for Public Health and the Environment. Physician diagnosis of COVID-19 was included as positivity because SARS-CoV-2 testing in the Netherlands was strongly restricted up until August, 2020.” Note that despite the limited testing and the known possibility of long COVID in asymptomatic and mild cases, no adjustment was made for those who were infected but not identified as such. Indeed the study reports an unexplained increase in the control group of long Covid associated symptoms of 18% compared to 29.6% in those that had identified infection. It is the difference between these numbers that they report as a prevalence of long COVID, at 13%. Moreover this study only looked at 23 somatic symptoms related to long COVID. Notably, they did not include psychiatric and cognitive symptoms that are known to be important and highly prevalent in long COVID. Had they included these symptoms, prevalence rates would have been higher. In the early days of the pandemic, it was common for prevalence studies to only include some of the symptoms now known to be related to long COVID. Another example is the first report from the Office of National Statistics in UK, that found a prevalence of lingering symptoms after COVID-19 of around 10%, a figure that was widely cited. Here, they only reported 12 symptoms.