(English translation of the German original)
The return to face-to-face teaching will only succeed if the three basic pillars of pandemic control are followed for the fall.
The concept behind this is called “Vaccinate-PLUS”.
Matthias F. Schneider, Technical University of Dortmund
VACCINATING AGAINST THE VIRUS is a race, and this race is far from over. We must continue to work against the virus to support the race in favor of the vaccination programs.
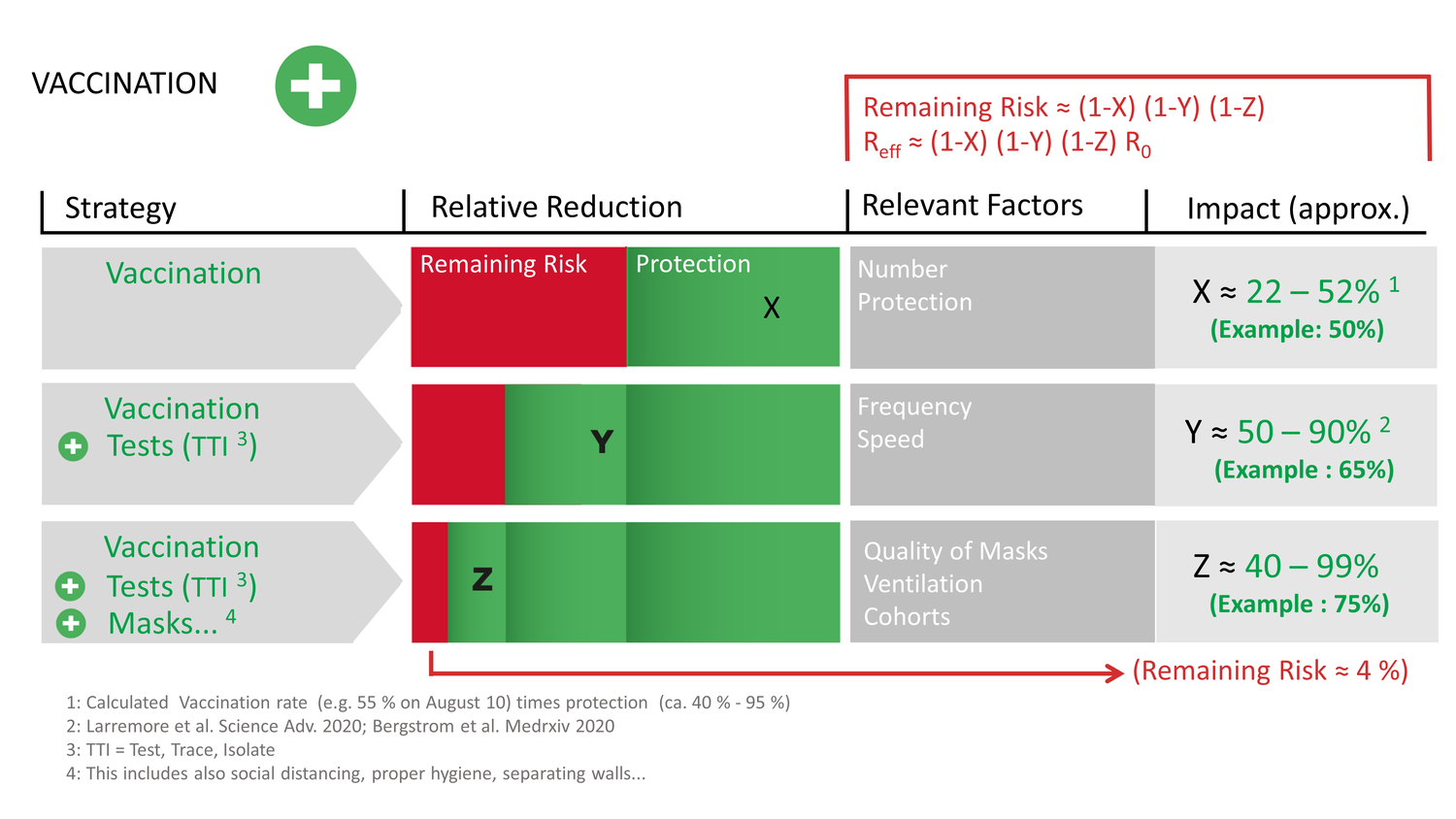
“Vaccinate PLUS NPIs” is the strategy, and it has three pillars: 1. vaccinate, 2. minimize exposure (including masks, air filters, and physical distancing), and 3. test – trace – isolate.
The entire concept works well and simple if you keep the numbers down. “Wait and see” is not a strategy and declaring the pandemic over is tantamount to ensuring that it will continue to trouble us for a long time to come. This also applies to universities and their plans for the fall semester. What is certain: careless openings prompt abrupt closings. A successful fall semester demands that we implement the three pillars of “Vaccinate PLUS NPIs”, and we do it this way:
1. Vaccinate. Since the situation in the fall/winter is difficult to predict, and the next wave has already begun and affects youth in particular, we should act now. On the one hand, by encouraging our students to get vaccinated, as is already being done in many places on campus. And on the other hand, by designing measures that can be used flexibly in parallel.
In the summer of 2020, the wave took off in the 15- to 30-year-old age group and spread from there. Waiting to see what happens means conducting experiments on the long-term effects of new variants on young people and children and risking further closures. Long- or post-COVID is a real disease with unpleasant consequences, also for the economy, not least because it affects the 18- to 29-year-old age group in the low double-digit percentage range (see Toolbox #10 of the NO-COVID Group). Additional measures not only ensure vaccination success, but also protect against the risk of so-called breakthrough infections among vaccinated people, which definitely occur with the delta or lambda variants, which are the dominant variants now (about two infected among 10,000 vaccinated versus 16 among 10,000 unvaccinated).

Matthias F. Schneider is professor of medical and biological physics at the Technical University of Dortmund. He is one of the founders of the No-COVID Initiative and a member of the multinational COVID Action Group (CAG). In the CAG podcast, he talks about how to open universities during a pandemic in “Community Elimination of COVID-19 and the Green Zone Exit Strategy – A Working Example“.
Even if a smaller proportion of those infected ends up in hospital, vaccination seems unlikely to protect against further transmission of the virus (at least for the delta variant). A large increase in infections (in both vaccinated and unvaccinated) may therefore at least partly neutralize the vaccination success. Therefore, a low-incidence strategy is also the only way back to normality for all those who cannot be vaccinated (for example, currently the ten million 0- to 12-year-olds in Germany) or those who have reduced vaccination protection for health or age reasons.
2. Minimize Exposure: masks, physical distancing, indoor air control. The N95-N100 masks are probably among the most efficient interventions: if two people in a conversation both wear an N95 mask during conversation, their improvement in protection is as good as after vaccination. So, mask up when indoors with others, even if recovered, vaccinated or tested. At least as long as the waning of protection from vaccines over time and against new variants is not clarified.
Another measure is working in small groups (forming cohorts). The reason for this is simple: if you have one infected among 100 students in a room, that person can infect a maximum of 99. If you divide the 100 into ten groups of 10 each, the one infected can infect a maximum of nine students in their group. From the community’s point of view, the risk of infection has thus been reduced by a factor of 11. If the meetings are spread out and scheduled wisely, the more limited contacts on the way to the university and on the campus (or school) are further reduced.
Additional protection can be achieved by smart ventilation concepts, for example with air filters that exchange the entire volume of the room several times per hour (see the DFG group’s new position paper). However, the frequently advocated ionizers should not be used. Opening windows to exchange air should be reconsidered against practicability and effect.
3. Test-Trace-Isolate. Masks, physical distancing and ventilation, however, do not tell you anything about the level of risk you are in. Therefore, the third intervention is a smart testing strategy. As long as sources of infection are still expected, testing prevents being blindsided. Testing means keeping your eyes open and remaining aware. This is as true on campus as it is at the airport.
If you find a positive case, you must immediately not only isolate it, but also aggressively “hunt” for the source, i.e., begin the (retrograde) contact tracing immediately. The reason is the physics of outbreaks, which teaches us that around ten percent of those infected cause 80 to 90 percent of infections. For the tracer, finding a positive case must be “celebrated” as it maps out a possible path to a superspreader, which are not easy to find otherwise.
Relying solely on pillar 1, vaccination, an effective R value of about 1.7 to 3.7 is achieved for the delta variant with a (rather optimistic) vaccination coverage of 80 percent and an R0 value of 6 to 8 (see figure). In other words: Vaccination alone will not end the pandemic even in the best-case scenario (high vaccination coverage and small R0). One needs the combination of all three pillars to enable further reduction (by about 60 percent on average) and keep Reff below 1. This strategy has further positive effects: Less risk of lockdowns as well as for vaccine breakthrough cases, and the long-term consequences (Long-COVID) will also be reduced. While keeping Reff below 1, booster vaccinations may be developed to prepare for the next round.
Implementation at TU Dortmund
On campus, all this is reasonably easy to implement. At TU Dortmund University, we therefore started to set up several PCR test lines in March 2021, where about 1500 to 2000 people per week were tested in pools of 10. The set-up, however, was designed to be scalable. Right now, we can already test about 10,000 people per week. In parallel, we are already testing alternative and additional methods for the fall semester: faster PCR methods (Quick-PCR), for example, and PCR tests on surfaces for so-called exit tests, tests performed after a class or meeting took place. The goal is to have a set of tools, adjustable to the situation, that is, to be able to test more if the incidence of infection is higher. A similar approach is taken with cohorting: following the precautionary principle, one starts with small groups at first and adjusts their size as the incidence in the region and risk assessment allows.
Thanks to the good communication with the local health department, tracking is handled with a minimum of red tape. In the event of a positive test, the university has a team that immediately begins tracing, provides the infected with the necessary information and works closely with the local health department. Speed is important, since every lost day in tracing means new infections, which starts a vicious cycle because more infections require more tracing… Each day puts additional strain on the system, slows down the processes, and the numbers go up even faster. Losses in speed of tracing require hard work to be compensated, e.g. by increasing testing frequencies or contact restrictions. Some publications have taken a closer look at this problem, which we also rely on in our science guided approach in Dortmund (see Toolbox #3 of the No-COVID group).
What do you have to do?
Just start, actually quite simple. At TU Dortmund, the president (a physicist himself) has shown the courage to follow the advice of science. The methods are not rocket science, and the concepts have long been published. However, the goals behind the concepts must be communicated well – including how you want to achieve them and the work they entail for the individual. And, of course, you must be aware of your role as a university. The strategy cannot only consist of demands – one has to offer something.
In addition to a reasonable testing concept, which has to include PCR tests, one must, for example, clearly signal that everyone is part of this. That is, you don’t just invite people to march into the testing center. But you also have to make it clear to those who have caught the virus, that by isolating themselves, they are doing society, and especially the campus community, a big favour, a favour that the university appreciates. Some of the signals we are sending out in Dortmund are, a well-equipped hotline, pick-up & shopping service for those who test positive and easy access to vaccination on and off campus.
Nothing is worse than waiting
The virus must be met proactively. If you wait, you will be controlled by it. Of course, as a university, we cannot directly determine what happens around us. But we can try to take advantage of our opportunities. On the one hand, we should make sure to have our clientele (i.e., especially our students) on board, educate them, start from where they are, and encourage them to get vaccinated, by providing easy access to the vaccine. At TU, we have already been able to offer a vaccination campaign on campus. Other campaigns will be organized as needed. We also continually highlight vaccination opportunities in the surrounding area: According to a recent survey, 92 percent of our students had already been vaccinated at least once by the end of July (compared to ≈ 60 % in the overall population of Germany), which is probably at least partly due to the good cooperation and communication between the university and students.
Minimal exposure concepts should already be available in universities of sufficiently good quality. However, it is also necessary to implement testing to be able to react fast, locally differentiated and with no regrets when outbreaks occur (see Toolbox #5 of the No-COVID Group).
With these three pillars (vaccination, minimal exposure, testing) it should be possible to carry out a reasonable semester, sustainably. After all, nothing is worse than uncertainty and on-off teaching.
In Dortmund, our concept on campus radiates into the city. For example, the TU Dortmund works not only with the local health department and the hospital, but also with the mayor, elementary schools and secondary schools, and is always available for questions and discussions. The Kids University explains to 7 to 12 year-olds what a pandemic actually is, and an information event was held at the Anne Frank School before the summer vacations, where students of all grades were able to openly ask scientists any questions they had about the pandemic. The event was recorded and made accessible for everybody.
The great potential of the university is, on the one hand, to impart and create knowledge. On the other hand, it consists of the many dedicated staff members and students who are easily motivated for a good cause. They are a superweapon in the fight against the pandemic. Use this superweapon so we can win the race against the virus and have a fall semester 2021/22 that can be planned. A fall semester robust enough to resist further variants and that can be recommended as an example beyond the universities.
Acknowledgement
The author would like to thank Angela, Julia, Vincent as well as Markus Beier and Yaneer Bar-Yam for their input and help with translation.


