Opening Schools Without Airborne SARS-COV-2 Mitigations is Violence Against Children, Parents, Teachers, and Communities [1].
by The Team at Shift Sight, September 2nd, 2021
Letter to a School
This is a pre-release with an open RFC. A PDF will be published shortly.
THIS LETTER IS AVAILABLE IN THE PUBLIC DOMAIN. ORIGINAL VERSION WAS PUBLISHED JULY 26th, 2021.
Dear Superintendent, Member of the School Board, Teacher, or Parent:
We are writing to you regarding the rapidly evolving situation around SARS-CoV-2 and COVID-19. You may be aware of the news around the Delta variant of concern (VOC), which is so contagious as to displace almost all other variants in the US. However, the scientific publications relate an even more troubling tale.
After recovering from COVID-19, permanent damage has been observed in approximately 1 of every 8 children. Individuals that met a clinical definition of “fully recovered” had reduced sizes in key brain structures and cognitive deficits. Worryingly, “the viral load in Delta infections are almost 1,000 times higher than those in the earlier [variant] infections,” increasing its ability to spread indoors. Most school protocols have been written with pre-Delta considerations. Transmission of Delta by fleeting contact has occurred at distances of 10-60 cm for mere seconds. As an airborne pathogen, Delta transmission has occurred from one individual to another simply by sharing indoor air hours apart.
School has not resumed everywhere in the US, and children are already in pediatric ICUs due to the Delta VOC. Some are over capacity. The head of the Children’s Hospital Association is pleading for immediate help.
In LA, 20% of recent cases are Delta breakthroughs in vaccinated people. Delta is not isolated geographically in the US.
We would like to request that you extend and encourage remote learning as a default for all families. For children that cannot attend remotely, a substantial amount of building mitigation is required to ensure a building is safe for occupancy against an airborne pathogen.
Children are at risk of neurological damage. If a building is not safe for children, it should not be open.
How can parents exercise good decisions about their children’s safety when it is not in their hands? Children need to be children. They need to be safe as well. No child should be disabled or die because we knew what needed to be done and failed to act.
This document is based on peer-reviewed scholarly literature and news reports given from state- and county-compiled data. The scientists, engineers, and professionals cited are leaders in their respective fields.
Actionable items are provided in the next section.
Thank you for your attention.
Respectfully,
The Team at Shift Sight
(For the purposes of this document, the terms airborne and aerosol are interchangeable. We reserve the right to retract and correct a statement if a factual error is discovered.)
Airborne Mitigations
1. Good engineering practice can facilitate a safe reopening of schools. ASHRAE has provided substantial guidance; their points are summarized here, with explanation provided in the appendix. An engineer must certify that these mitigations are properly implemented. ASHRAE is available to answer your questions via COVID-19@ashrae.org.
2. A first step to controlling transmission is to reduce the opportunities. When considering the infectious potential of the Delta variant of SARS-CoV-2, this translates to remote learning. Remote learning prevents transmission and infection and keeps children out of hospitals. Beyond reducing opportunities for infection, building mitigations and personal protective equipment (PPE) are required to control transmission as the current vaccines are non-sterilizing.
3. For students that must be present at school, the strategy must focus on airborne mitigations and PPE:
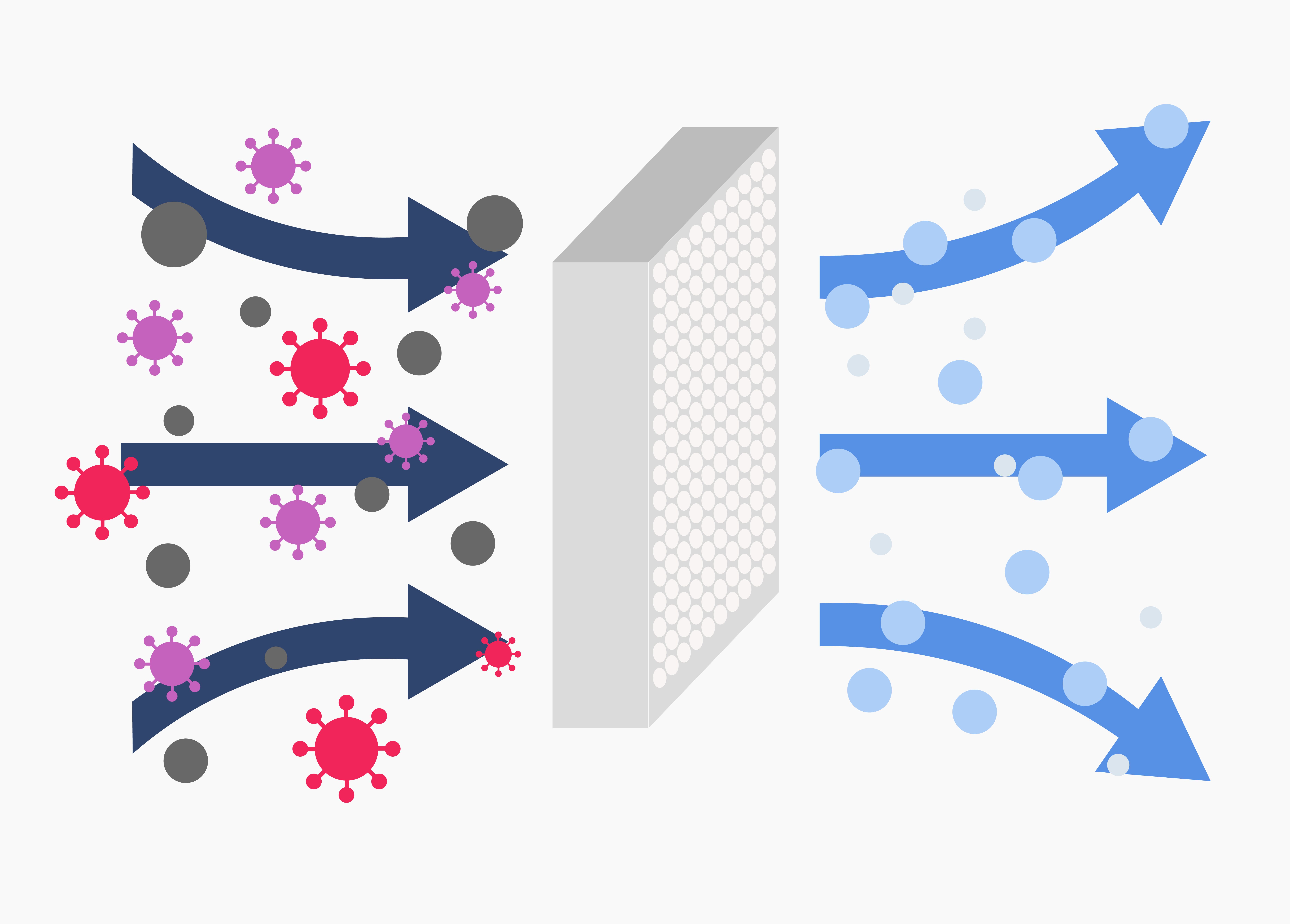
3a. Filtration: Just as cities provide clean water, schools need to provide clean air. Per ASHRAE, MERV 13 filters should be installed in school HVAC units. The possibility of finer aerosols in a school (singing) suggests up to MERV 17, but the HVAC unit will need to be evaluated for suitability with the pressure drop. As a secondary benefit, children perform better academically in schools with proper filtration.
3b. Air Change Rate: Airflow is important to prevent SARS-CoV-2 from concentrating in localized areas of classrooms. It is suggested that school buildings should be able to provide 6 air changes per hour (ACH) for each classroom at a minimum for Delta. An engineer will need to evaluate the HVAC motor performance and building to establish ACH.
3c. Localized Filtration: Air cleaners with HEPA filters (not “HEPA-type”, “air cleaners”, or “ionizers”) reduce localized viral loads while increasing total ACH. (HEPA filters may be treated as MERV 16+ equivalents.) Cleaners should provide a sufficient clean air delivery rate (CADR) for the size of room and must be operated at the rated fan speed. An engineer will need to evaluate how these influence overall building air change rates. If HEPA cleaners are too expensive, a DIY Corsi/Rosenthal Box may be used provided the local jurisdiction does not strictly require UL-certified products. (DIY air cleaners, in general, were evaluated by UL with no concerns.) Ultraviolet light (UV), occasionally built into HEPA air cleaners via a UV bulb, cannot be endorsed since low-cost UV bulbs emit undesirable wavelengths that will produce ozone and can negatively influence indoor air quality (IAQ).
3d. Ventilation: Poorly ventilated spaces are attributable to airborne SARS-CoV-2 transmission. Indoor air should be exhausted to atmosphere periodically and replaced with fresh air. A continuous exhaust to atmosphere will reduce airborne pathogens. UV light from the sun sterilizes the air after a period of time, but care needs to be taken that one room’s exhaust is not another room’s immediate intake.
3e. CO2 Monitoring: Ventilation rates may be established with real-time CO2 monitors in occupied classrooms. CO2 is not a direct surrogate for IAQ or infectious aerosols but can indicate if ventilation is sufficient for occupancy level and activity. (Exercise, for example, would produce more CO2 and aerosols, requiring more ventilation if the room size is the same.) Excessive levels can be used as an alarm to move a classroom outdoors. Note, however, that CO2 will not track with infectious aerosols with HEPA cleaners running. Monitors should be placed at about children’s mouth level and must use outdoor levels (local) as a baseline.
3f. FFP2/KF94/KN95/N95/Elastomeric Respirators: Respirators reduce the inhaled aerosol concentration by up to 72% without localized HEPA cleaning. All building occupants should wear one regardless of vaccination status. When a hospital upgraded the staff PPE in COVID-19 wards, there was a 100% decrease in hospital-acquired SARS-CoV-2 infections among staff. (It is imperative to keep people out of hospitals; in Wales, 25% of the COVID deaths are after being “definitely” or “probably” infected with SARS-CoV-2 in a hospital setting.) Respirators are not interchangeable with cloth or surgical masks, and must be certified to remove 94%+ of airborne particulate matter down to 0.3 microns. Respirators must seal properly and should never be removed while indoors.
3g. Relative Humidity (RH): As ventilation brings outdoor air inside, it may increase the RH in classrooms where high outdoor humidity is present. Although SARS-CoV-2 is shown to spread more easily at lower humidity, high humidity can create the potential for mold and related health hazards. HVAC operation in these circumstances requires specific considerations to maintain humidity, including DCV operation.
3h. Maintenance: HVAC filters, HEPA filters, and filters in a Corsi/Rosenthal box need to be replaced periodically. Permanent HEPA filters exist and may be useful for financial constraints, but the accompanying instructions need followed carefully (with appropriate PPE) to ensure the individual cleaning a filter is not infected. Unless elastomeric, respirators should not be washed or reused since this can damage their electrostatic properties.
3i. Outdoor Snacks and Lunches: With the increased infectious nature of Delta, there is no such thing as a safe indoor meal. Children should be outdoors, spaced at least 15-20 feet apart, or what would be considered acceptable for a distance between an asthmatic child and a smoker. (Although infectious aerosols do not travel identically to smoke, they have approximate behavior for this discussion.)
3j. Minimum Occupancy and Cohorts: Reducing class sizes by alternating between in-person and remote learning days will enable 1) reduced community spread, and 2) fewer students quarantined in the event that some mitigation should fail and a positive case is identified.
3k. Limited Reliance on Tests: Delta, AY.4, Lambda, Mu, and other variants occasionally result in false negatives depending on the test and when it is administered relative to exposure. Therefore, any symptoms should be treated as suspicious and a positive case; if a child became ill with these airborne mitigations in place, it is pragmatic to treat it as a SARS-CoV-2 infection and quarantine the cohort.
3l. Treat All as Unvaccinated: The vaccines do not provide sterilizing immunity that would stop infection and community spread. A vaccine is not PPE, nor is it a replacement for NPI or PPE. All occupants need to follow these requirements identically regardless of vaccination status. This also protects immunocompromised children.
3m. Classroom Seating: No child should be able to exhale directly into another child’s face. Near-field aerosol concentration is substantial, and a poorly-timed failure of a respirator seal can lead to an infection regardless of classroom ACH and ventilation rates.
4. Keeping children safe from a highly infectious, airborne pathogen that has long-term consequences requires extensive vigilance, NPI, and PPE. If these requirements cannot be implemented, your school should not be open. It is a danger to children. Remote learning is the easiest and most sensible way to keep our communities safe.
Appendix
Droplet vs. Airborne Transmission
5. Policy in the US has centered on a droplet theory of transmission. Research confirms that SARS-CoV-2 spreads primarily through airbornetransmission mode. The US CDC has made this concession in recent months but retains guidelines for droplet. Airborne spread requires the mitigations presented.
6. As background, droplet transmission is partially described by Stokes’ law, stating that droplets expelled by an individual will travel a finite distance before settling on the ground or surfaces. Droplets “drop.” This has been the basis of social distancing despite no supporting research: “6 feet” or, inexplicably, “3 feet in schools” because “it will make it much more feasible for many schools to open”. With airborne transmission, there is no safe distance indoors.
7. In an airborne transmission model, the particulates expelled from an individual are fine and diffuse into the local atmosphere according to fluid dynamics. In one case, a COVID-positive individual infected someone 15 meters behind them. One can visualize every exhale from every person in a room as a smoke that mixes. SARS-CoV-2 virions maintain their infectious properties for hours in air.
8. ASHRAE is an engineering society whose members are concerned with the safeguarding of life and health in buildings. ASHRAE has described airborne transmission as a primary means of infection since January 2021, later affirming that airborne transmission of “SARS-CoV-2 is significant and should be controlled.” Their recommendations are actionable by all buildings and are especially applicable to school situations of concern by the CDC.
9. Conclusions: SARS-CoV-2 is transmitted primarily by airborne means. Policies focused on droplet transmission are insufficient for the safeguarding of life and health. This is observed internationally where a UK school session had 400,000 children miss school in one week due to SARS-CoV-2; it is observed in the US as schools open for days and then close due to outbreaks. Each outbreak carries the risk of permanently disabling or killing a child.
Personal Protective Equipment (PPE)
10. The CDC initially recommended masking at the start of the pandemic. Medical-grade masks prevent transmission by droplet. Unfortunately, SARS-CoV-2 does not transmit primarily by droplet, and these masks are not rated to filter aerosols. If surgical masks are your only available choice, they can offer limited protection with a mask brace to improve the seal. Do not reuse them. Fresh masks contain electrostatic properties that can attract and trap airborne particulates. As time passes, the high relative humidity (RH) of exhaled air continuously degrades the electrostatic properties and gradually changes the mask to a biological substrate. (This is most noticeable to the wearer as a bacterial odor and is a clear indicator of an exhausted mask.)
Aerosol reduction properties of masks that are not respirators. Charts do not reflect the risk of Delta.
[Image is part of https://pubs.acs.org/doi/pdf/10.1021/acs.est.1c00235, reproduced here as Fair Use per 17 USC § 107]
11. Respirators are another form of PPE. Medical professionals involved with aerosol generating procedures (AGPs) are required to use NIOSH-compliant respirators, such as an N95, to prevent spreading disease. Allowing that airborne SARS-CoV-2 infection from 15m (49 ft) away indoors has been demonstrated, N95 respirators or equivalent should be the minimum PPE considering that human activities produce aerosols of varying size [and corresponding virulence] beyond the AGPs listed by the CDC. Singing, for example, produces finer aerosols (more potentially infectious surface area) in a higher quantity per second.
12. Although not a primary consideration, SARS-CoV-2 community transmission may further be inhibited with eye protection such as face shields.
13. Conclusions: The CDC mandates respirators for AGPs. Properly-fitted N95 respirators (or elastomeric equivalents) should be the minimum PPE for controlling the airborne spread of SARS-CoV-2.
Vaccination and Transmission
14. Vaccinated individuals are not exempt from the recommendations in this document. Unfortunately, the current vaccines do not provide sterilizing mucosal immunity. Vaccinated individuals carry and transmit SARS-CoV-2 by nasopharyngeal shedding. This was confirmed in Singapore, where contact-tracing and genomic sequencing of an outbreak gave a precise picture of disease transmission:
Disease transmission. [Image taken from https://covid.viz.sg, reproduced here as Fair Use per 17 USC § 107]
Green = Fully Vaccinated, Yellow = Partial, Gray = None
15. In the example above, transmission occurs regardless of vaccination status. This is the scenario of young children returning to school with a vaccinated teacher. Appropriate non-pharmaceutical interventions (NPIs) outlined thus far should be the foremost consideration ahead of vaccination status. This is akin to a zero-COVID elimination strategy, championed by some groups such as Independent SAGE.
16. With Delta, a study involving 719 people identified that vaccinated individuals can be infected and transmit viral loads at a rate that is identical as unvaccinated individuals. Furthermore, vaccinated healthcare workers (HCWs) may shed SARS-CoV-2 for up to 32 days after infection. Delta is also spread by people “that feel fine,” shedding virions for up to 2 days prior to symptoms. It should be fully understood that a vaccinated teacher does not protect unvaccinated / vaccinated students or their families. NPI and PPE are required.
17. Public messaging around vaccination has been overly simplified to a binary, static state: did you get your shot or not? This is a dangerous oversimplification. Vaccination confers immunization to varying degrees, and personal immunity is a dynamic, individual, and situational response that varies with time. For example, “roughly 10 million [vaccinated] Americans whose immune systems are compromised […] may not be well protected.” Breakthrough infections are probable in the general population and guaranteed among immunocompromised (IC). Breakthroughs are possibly being undercounted.
18. Conclusions: Vaccination does not negate the use of PPE and NPIs. Vaccine efficacy (VE) was taken from studies as a static, mathematical average of a population in a specific situation. Public officials dangerously presented this static number as a guarantee for all circumstances in all individuals. (It remains to be seen if VE was overstated by NPI, as everyone in the phase III trials were masked and cautious.) The biological reality is that VE, for a non-sterilizing vaccine, is highly situational and may be modeled as a real-time, complex, dynamic system with no guarantees.
Delta, Long-COVID in Children, and Variants of Concern (VOCS)
19. The pandemic today is not the same as one year ago. Delta (B.1.617.2, first identified September 2020 prior to vaccine rollout) is a primary variant of concern. (AY.4, of Delta sublineage, is spreading faster.) Due to Delta’s excessive viral load, it spreads easily regardless of vaccination status. In one instance, a vaccinated individual was able to transmit Delta to 83 peers in one setting. An outdoor music festival generated thousands of Delta infections. In Israel, a recent news report indicates that 60% of patients in serious condition are vaccinated. Delta now comprises more than 99% of all new cases in the US.
20. A comprehensive study has recently concluded that COVID-19 is more accurately described as a post-viral autoimmune condition rather than an acute respiratory condition. Long-COVID can present as a devastating chronic condition in children with no known treatment for the constellation of symptoms. In 3,762 people across 56 countries, a study has identified over 203 different symptoms across 10 organ systems. In one study, a fifth of asymptomatic individuals went on to develop long-COVID. A study lasting 6 months showed 61% of patients had persistent debilitating symptoms that were independent of the severity of the initial acute illness. A preprint indicates vaccines do not prevent long-COVID.
21. The risk to children cannot be understated because the risk is not fully understood. In some children, SARS-CoV-2 may function as a superantigen and produce symptoms similar to MIS-C. Up to a million people may already suffer from long-COVID, and some children are now wheelchair-bound. Long-COVID is serious and potentially a permanent disability with no treatment. Sequeale and long-term effects of SARS-CoV-2 are unknown. In one study, every child that was infected had elevated biomarkers suggesting blood vessel damage.
22. In the states, the focus has been on hospitalizations and death rather than medium- and long-term effects. As a result, official statistics have severely undercounted pediatric cases, possibly up to 13-fold (9,044 vs. 117,805) in at least one region. Just because a child does not end up hospitalized at onset does not convey any correlation to long-term health.
23. There are other VOCs in the US, including Delta+, Lambda, and AY.4. We can expect more and new variants, including those with features that contribute to vaccine evasion. A study has suggested that while naïve and convalescent individuals pressure random SARS-CoV-2 mutations, vaccinated individuals dampen genomic diversity since the vaccines do not prevent infection. This implies that spreading Delta through a community, leading to breakthroughs, will intentionally create immune evasion.
24. Conclusions: With Delta and AY.4 circulating, children are guaranteed to get infected in a school setting unless proper mitigations are in place. Every infection carries some degree of permanence. Some of those children will be disabled due to long-COVID. The risk to all children, teachers, and parents cannot be understated. Immunocompromised teachers and students are especially at-risk
Opening schools without airborne SARS-CoV-2 mitigations is violence against children, parents, teachers, and communities. https://www.shiftsight.com/covid-statement.html