Accuracy of Excess Mortality Statistics Under Threat in UK
Over the course of the COVID-19 pandemic, governments around the world have minimized the perceived severity of COVID-19 by adjusting how pandemic data are measured and presented. For example, reducing the availability of PCR testing, alongside irregular reporting of PCR positive cases, has allowed for the appearance of “declining” cases. At the same time, the under-reporting of deaths after COVID-19 diagnosis by omitting COVID-19 infection in the reported cause of death has given the impression that deaths from the disease are “decreasing.” With testing metrics no longer reliably accurate, one of the final tools we have to trace one of the most serious effects of COVID-19—how many deaths are caused by it—is excess mortality data. Yet even this tool is now being compromised after certain governmental organizations, such as the UK Office of National Statistics, are now recalibrating how they obtain this number. By doing so, they are artificially lowering the numbers of excess deaths, and contributing to misinformation on the true impact of COVID-19 on the population.
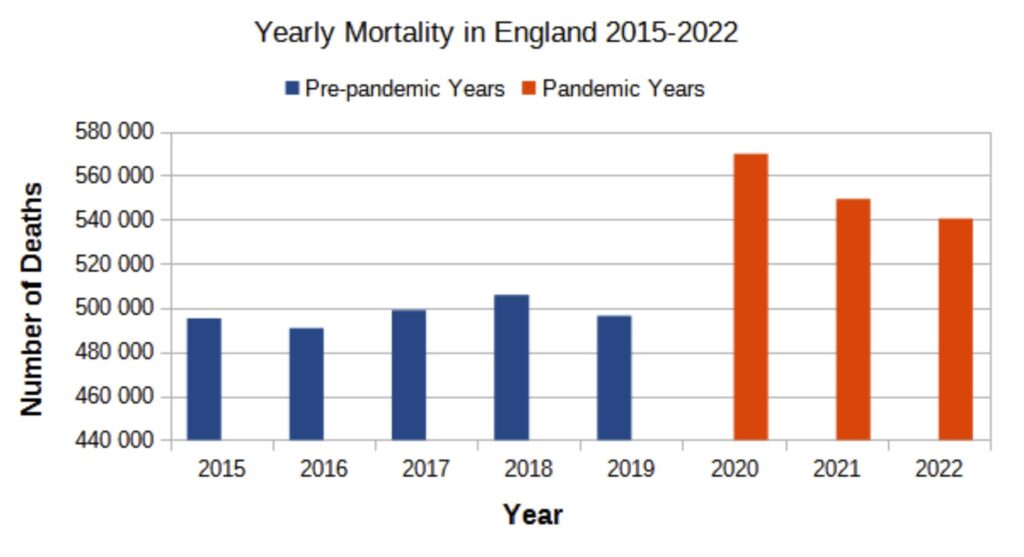
The method of calculating excess mortality related to an event is generally straightforward, comparing the number of deaths that took place during the event with the mean mortality rate across the five years prior to that event1. Aligning with this approach, measures for excess mortality related to the COVID-19 pandemic (the event) have incorporated the five-year period prior to the pandemic (2015-2019) as part of the baseline measure for excess deaths. However, the UK Office of National Statistics (ONS) has announced plans to begin including pandemic years into its baseline mortality calculation. Although the ONS is continuing to exclude 2020 from the mortality calculation as a ‘pandemic year’, it will begin incorporating 2021 and 2022 into the baseline mortality measure in the March 2023 edition of “Monthly Mortality Analysis, England and Wales”3. It is crucial to note that 2021 and 2022 are also definitively ‘pandemic years’, in which the spread of the SARS-COV-2 virus around the world caused mass infection, multiple new variants, and continuing elevated excess mortality above 2015-2019 levels 4,5 (Fig. 1). The ONS’s change in policy to begin including 2021 and 2022 in their excess mortality calculations has understandably been met with skepticism and questions into the integrity of this statistic moving forward.
The ONS’ decision to change their baseline measure for calculating excess deaths to account for the COVID-19 pandemic, according to an official blog post, was driven by the following questions6:
- “Are we trying to calculate the number of deaths had there not been a pandemic, that is to say estimate the impact of the pandemic on mortality?
- “Or are we trying to calculate the number of deaths given there has been a pandemic, i.e. to inform us about what is happening now?”
If the goals were aligned with question 1, the measure for excess mortality would use only pre-pandemic years as the baseline, making the excess mortality associated with the COVID-19 pandemic more evident. In contrast, measuring excess mortality in accordance with question 2 would incorporate excess mortality as part of a new baseline measure and is a step towards normalizing a level of death that, prior to the pandemic, was considered unusually high (e.g. “excess”).
The ONS reported excess mortality for March 2023 of 5679 people, or 12.6%,3 suggests the ONS chose to focus on answering question 2 to inform us of the mortality given COVID-19 exists—the implication being that its existence is no longer unusual or worthy of the “pandemic” label. If ONS had instead used only the pre-pandemic years in their calculation, 2015-20197, the reported excess mortality for March 2023 would have reflected a higher burden of excess death–6,009 people (13.4%). This may not seem like a major difference when examining data for a single month, March, but examining the differences in total excess death using the two methods to examine deaths for several months per year makes the difference more apparent.
For example, combining the January-May data from 2017-2019 and 2021-2022 yields an average mortality of 245,249 people. For 2023 ONS reported 263,812 deaths total in the same five months, meaning the excess mortality in England for the first 5 months of 2023 would total 18,563 deaths, or 7.57%7. In contrast, the average mortality for January-May of 2015-2019 that excludes pandemic years, 238,712 deaths, is much lower. The result yields higher excess mortality for the first 5 months of 2023, a total 25,099.8 deaths, or 10.51%7, which is larger by almost 40%.
The ONS approach excluding only one pandemic year points to another possible explanation for the new ONS method of measuring excess mortality: they want to reinforce the idea that there was only one bad pandemic year, 2020, in the past.
However, the data do not support the notion that 2020 was the one sole pandemic year, nor that the pandemic is in the past. The total mortality in England in 2021 and 2022 is significantly elevated compared to pre-pandemic years, and more closely resembles the mortality data from 2020 than the period from 2015-2019. (Fig. 1). Excess mortality in 2023, measured using exclusively pre-pandemic mortality rates, remains substantial2, and directly threatens the ‘pandemic is over’ narrative, as do the high levels of mortality in the second and third years of the pandemic.
The incorporation of 2021 and 2022 into baseline mortality statistics artificially inflates the baseline number of deaths (the denominator) and underestimates ongoing excess mortality. This manipulation of statistics achieves a short-term goal currently being pursued by many Western governments —obscuring the impact of COVID-19 on excess mortality to normalize the continued spread of the virus, minimize the severity and impact of infection on individuals and communities, and sell the idea of returning to the pre-pandemic status quo even though it is continuing. Enabling this ‘return to normal’ narrative comes with serious long-term trade-offs. Most importantly, the narrative itself contributes to the increase in infections and mortality. Incorporating the excess rates of disability and death being caused by COVID-19 into baseline public health statistics, will make it more difficult for policy makers to correctly assess and deal with the long-term impacts of COVID-19 on the population.
If the ONS continues to use this proposed approach, the ongoing excess mortality caused by COVID-19 will be integrated into the baseline mortality statistics within a few years. If the changes continue, in 2024, data from 2023 will replace data from 2017, and by 2026, the baseline will be calculated using data from 2021-2025 – thereby exclusively reflecting mortality of the COVID-19 pandemic. The ongoing excess mortality from COVID-19 would become the “new normal” – and does so with little public awareness. Instead, the ONS has opted to use an obscured technical change to limit the public’s access to one of the few remaining sources of information that illustrates the true risk posed by the ongoing pandemic.
The ONS’s change in how it calculates excess mortality data will have downstream effects on the policies enacted by other government agencies and decision-making bodies in the UK, which rely on COVID-19 data from the ONS to assess the risks posed by the virus. With less data supporting the idea that COVID-19 is an ongoing threat – a claim that persistently elevated excess mortality data supports – policy-makers will have little motivation to pursue policies that acknowledge the risks of COVID-19 transmission, or try to address the multitude of downstream ill effects caused by the continued spread of COVID-19. These same statistics will be picked up and used by mainstream media outlets to shape the ongoing pandemic narrative that COVID-19 no longer poses significant risk8 – and anyone seeking to refute this narrative will have limited publicly-visible data to support their argument.
As the fight to define the narrative of the pandemic goes on, the behind-the-scenes changes in how governments are calculating statistics such as excess mortality will almost certainly become hidden. However, manipulating how the excess deaths caused by the ongoing spread of COVID-19 are measured does not, in fact, make them go away.
Yet, 2023 is still showing substantial excess mortality. In England, March of 2023 had the highest mortality numbers since the start of the pandemic3,7.
It’s as if the COVID-19 pandemic was still raging…that is to say, it’s quite clear the pandemic is ongoing.
References:
1. Checchi, F., & Roberts, L. (2005). Interpreting and using mortality data in humanitarian emergencies. Humanitarian Practice Network, 52 as quoted in https://ourworldindata.org/excess-mortality-covid
2. See https://www.euromomo.eu/graphs-and-maps for an example of 2023 excess mortality in Europe.
6. https://blog.ons.gov.uk/2023/02/10/how-do-we-measure-expected-and-excess-deaths/
9. https://www.mirror.co.uk/news/health/brits-dying-tens-thousands-dont-29955386
All sites consulted on the 12th/May/2023


