I Feel Lousy: Could This Be Long COVID?
In the aftermath of COVID-19 infections—even if you weren’t aware of having one—many people find themselves grappling with lingering symptoms that don’t quite add up. You may feel fatigued, struggle with brain fog, experience shortness of breath, or notice a rapid heart rate after minimal exertion. If you’ve asked yourself, Could this be Long COVID?—you’re not alone.
What Is Long COVID?
Long COVID, also known as Post-Acute Sequelae of SARS-CoV-2 (PASC), refers to a range of symptoms linked to underlying physiological harm that persist after the acute phase of a COVID-19 infection has resolved. While COVID-19 is often thought of as a respiratory illness, the infection impacts blood vessels and many tissues, with effects that can persist in multiple locations in the body. This means that COVID-19 is a systemic disease, affecting multiple organs and bodily systems.
Long COVID symptoms can include, but are not limited to [Find a more comprehensive list of Long COVID symptoms here]:
- Fatigue: Unrelenting, debilitating tiredness that doesn’t improve with rest.
- Brain fog: Difficulty concentrating, memory lapses, and confusion.
- Breathing issues: Persistent shortness of breath or chest tightness.
- Heart problems: Palpitations or a rapid heart rate.
- Muscle and joint pain: Unexplained aches and stiffness.
- Neurological symptoms: Headaches, dizziness, or sleep disturbances.
- Gastrointestinal issues: Nausea, diarrhea, or abdominal pain.
- Immunological issues: Vulnerability to other infections, and heightened sensitivity to allergens or new allergies.
- Emotional challenges: Anxiety, depression, or atypical mood swings resulting from neurological and physical damage.
Who Can Get Long COVID?
Anyone who has had COVID-19—whether asymptomatic, mild, moderate, or severe—is at risk of developing Long COVID. Approximately 50% of acute-phase infections are asymptomatic, meaning many people with Long COVID never knew they had COVID-19 in the first place.
Long COVID does not discriminate. It can severely impact people of all ages, including those who are athletic and highly active, leading to profound changes in physical abilities and reshaping their expectations for daily life.
How Do I Know If It’s Long COVID?
If you’re experiencing surprising symptoms that persist or are medically urgent, it’s worth considering Long COVID. Key questions to ask yourself include:
- Are these symptoms interfering with your daily life?
Long COVID symptoms often disrupt normal activities, making it hard to work, exercise, or handle basic tasks. - Do these symptoms fluctuate?
Many people with Long COVID report that symptoms come and go or worsen after physical or mental exertion (a phenomenon known as post-exertional malaise).
What Should You Do?
If you suspect Long COVID, it’s important to take proactive steps:
- Talk to a Healthcare Provider: Share your symptoms and medical history with a doctor familiar with Long COVID. Bring notes on when your symptoms started and how they’ve progressed.
- Seek Specialist Care if Needed: Long COVID may require a multidisciplinary approach, involving cardiologists, pulmonologists, neurologists, or other specialists. They will each treat the issues that they are able to, but there is no specific treatment for Long COVID.
- Track Your Symptoms: Keep a journal of how you feel daily, noting triggers that worsen your symptoms. This can help your healthcare team tailor a management plan.
- Rest and Pace Yourself: Avoid overexertion, as it can exacerbate symptoms. Focus on gradual, gentle activity rather than pushing through fatigue.
- Explore Support Networks: Long COVID is not just a medical condition—it’s also an emotional and social challenge. Joining support groups or communities can provide understanding and shared experiences. These groups are also sharing insights about how to improve your condition or accelerate recovery, including the importance of avoiding exercise until you are ready.
Why Recognizing Long COVID Matters
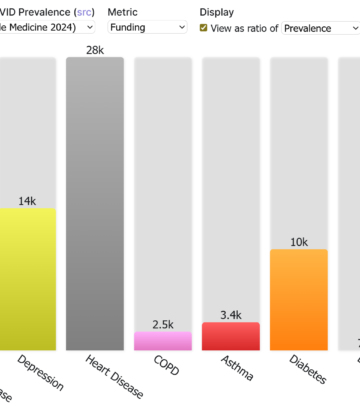
Despite tens of thousands of scientific papers on Long COVID, some still claim that it is “in your head.” This is not the case. It results from physiological changes in your body due to COVID infections, and it affects millions worldwide. COVID infections can cause organ damage, which also raises the probability of heart attacks, strokes, and other sudden problems that can be life-threatening. Addressing risk factors that can contribute to these life-threatening problems early is essential to prevent severe outcomes.
Recognizing and addressing Long COVID early can improve your quality of life and help guide researchers and healthcare providers in creating better treatments.
If you’re feeling lousy and wondering if it could be Long COVID, you deserve answers and care. Trust your instincts, seek medical advice, and remember—you’re not alone. Together, we can support each other and navigate these challenges toward recovery.