High Risk Institutions
Introduction
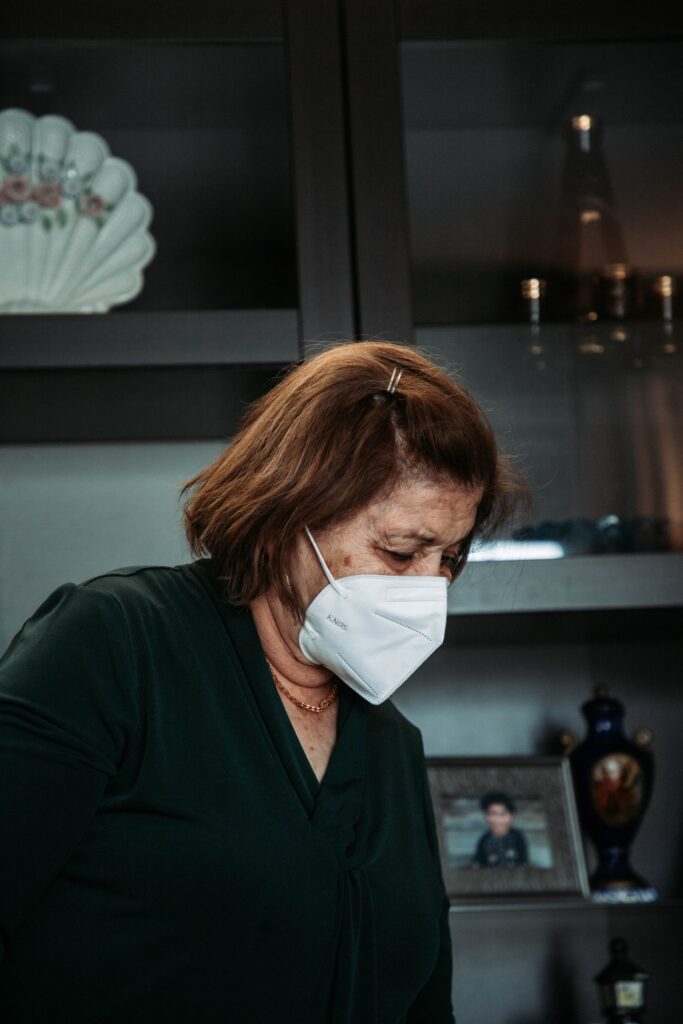
Long-term care institutions, nursing homes, care homes, assisted living and retirement homes are high-risk institutions for disease transmission because residents are vulnerable due to their health status and their close proximity to one another. COVID-19 is a rapidly transmitting disease requiring hospitalization in about 6% of cases and resulting in death in 2-10% of cases in these high-risk settings. Complications further increase for persons 70 years old and above with pre-existing comorbidities especially heart failure, diabetes and hypertension. COVID-19 can transmit with mild symptoms (coughing, sneezing or elevated temperature) and even through asymptomatic persons unaware that they are infected. Reducing the likelihood of transmission is imperative in high-risk institutional environments as has been clearly shown initially in China and subsequently in European and American outbreaks.
Although the number of deaths from COVID-19 in care homes varies between and within countries, the percentage of COVID-related deaths in care homes worldwide range from 24% to 82% [1]. This policy snapshot looks at what countries have done to protect care homes during the COVID-19 crisis, including providing guidance, strengthening medical support, testing for residents and staff, and other supportive measures.
Here are recommended guidelines for prevention by introducing barriers to transmission from outside a facility, managing internal processes and helping the workforce to care for and protect residents [2]. Developing guidelines is an ongoing effort, we summarize the main suggested strategies to deploy and highlight key items to take into account as of today.
The document is divided into sections. Section 1 covers rules for visitors, testing and outbreak monitoring, hygiene, dining and other high contact activities, employees and corporate environment, air quality and records. Section 2 covers enhanced rules for areas of active transmission regarding visitors and testing, dining and other high contact activities as well as employees, facilities and corporate environment. Section 3 lists a series of measures taken in some states and countries leading to distinct success in protecting care homes residents. Appendices cover A) employee safety and screening questions, B) Personal protective equipment (PPE), C) Definitions of COVID-19 cases and contacts, D) Isolation of confirmed, suspected or symptomatic residents, E) Receiving residents being discharged from hospital and F) Decontamination and cleaning processes for care homes with possible or confirmed cases.
General Rules
In the last four months, the medical and scientific communities and the Endcoronvirus.org team have examined measures different countries have taken to protecting care homes. The data we have obtained is consistent with basic principles on how to achieve robust prevention and risk reduction. In order to continue to improve, it is important to identify approaches that have led to better outcomes and to draw out learning for the ongoing and future outbreaks. Prevention and control systems and emergency plans should be developed. Strict management of movement in and out of centers, health monitoring for early detection of COVID-19 cases and quarantine and segmentation plans have shown to be important. In addition, studies found that caregivers working in multiple facilities leads to more cases and higher death rates (notably see [3]).
In order to respond in a timely way to the COVID-19 pandemic in high-risk Institutions, it is important to enhance risk control strategically, as well as strengthen daily prevention and control measures such as personnel protection, environmental cleaning, and disinfection. Mitigation strategies that will be addressed: 1. Visitors; 2. Testing and outbreak monitoring; 3. Hygiene; 5. Dining and Other High-Contact Activities; 6. Employees and Corporate Environment; 7. Air Quality; 8. Records.
Visitors
- Discourage non-essential visitors. Note: an essential visitor is defined as necessary to the resident in terms of maintaining mental and/or physical health, or is required in specific situations including end-of-life, change in health status or other pressing or important circumstances (e.g. financial or legal matters, family crisis).
- Determine clear guidelines about conditions and behaviors for which visiting is not allowed including symptoms, travel, mask-wearing, occupational risks, and so on. Inform staff and residents about these guidelines. Specific conditions depend on the settings and the resident types. Examples of visiting conditions include:
- Indoor visits conditions:
- Each resident or alternate decision maker may designate one Family/Support Persons (over the age of 18) or up to two if it is essential to maintaining mental and physical health.
- Additional visitors may be given access in specific situations including end-of-life, change in health status or other pressing circumstances (e.g. financial or legal matters, family crisis).
- Outdoor visits conditions:
- Up to four individuals, including the resident, may participate in outdoor visits, with distancing requirements, if consistent with site policy and public health measures.
- Position someone at entrances to query the purpose of the visit and ask if the visitors have any symptoms, have recently travelled to areas of active transmission, or have been exposed to people with symptoms as well as proceeding with scanning temperature of the visitors. Note: This must be communicated clearly before visitors arrive at the location, only to potentially be turned away at the door.
- Provide a questionnaire for those at entrances:
- Symptoms that were present during 14 days before.
- Do they live with other people and if so ask about symptoms of household members (they may be asymptomatic but the people living with them could be symptomatic).
- Ask about travel in the last 14 days to identify the risk level of the locations of travel.
- Do they work with infected or high-risk people in their jobs (doctors, nurses, …).
- Ask them to notify if they experience symptoms within 14 days after the visit.
- Keep a log of all visitors with contact information and in times of higher risk call them after the visit to determine if they subsequently have symptoms.
- Require wearing masks or face covering for each entering visitor. N95 masks are advised when possible for the visitors or if the facility can provide them.
- Visiting should be spaced at intervals to avoid crowding. Online appointments are suggested to simplify the process and reduce the risks of overcrowding the entrance pre-screening.
- Best practices guidelines should be posted in an easily readable format and relevant languages in public spaces for employees, residents and visitors to see.
- Have a designated area for visiting. Ideally, this area should have direct access to the entrance so visitors do not have to pass by various parts of the facility & should be cleaned & ventilated as often as possible (best after each visit) and having a hand sanitiser and mask station at entry.
- Spare rooms in the facility should never be used as quarantine housing for potential/positive cases.
- Outdoor visiting is a safer option, weather permitting. These also have to be scheduled so there is not overcrowding. Tables, chairs and other outdoor equipment must be cleaned between visits.
- In times/regions of high community transmission, all visits should be prohibited except for an emergency.
- Provide for and facilitate alternate means of maintaining family contact – Zoom, Skype, assisted phone calls, etc., appropriate to the setting.
Testing and outbreak monitoring strategies
- Educate staff and their families, as well as residents and their families, about coronavirus transmission and prevention. Ensure employees know that when they have even mild symptoms they should not be at work locations or in-person meetings and they will be paid and not penalized for sick days. Set up a reporting system for any cases (see Appendix A for a suggested “Employee Safety and Screening Questions for Employers”).
- Ensure employees have appropriate health insurance policies so that they will not be afraid to seek out care when they have symptoms, even mild ones.
- Ensure a proper and continuous supply of PPE for the workforce (see Appendix B for more info on PPE). Document proactive contingency plans for temporary PPE supply-chain interruptions. Eye protection (face shields or goggles) is to be encouraged along with masks or other face coverings (not as a substitute for masks). As a supplementary preventive measure, consider making masks or other face coverings available for workers’ families and household members.

- Targeted random sampling of staff and residents: In a regular (non-active) setting this way of testing, diagnostic or tests (DNA tests, qRT-PCR tests or possibly viral RNA tests or even the use of regular screening with pulse-ox meters where possible) as a further aid), are applied to individuals of high risk populations, for example, in confined communities such as nursing homes, rehabilitation facilities, psychiatric wards, medical facilities, or retirement communities. In those locations when one individual is infected many individuals are likely to be infected even if they are not yet showing symptoms or would have positive test results. In that case, the entire community can be isolated as individuals.
- Mass Screening: Systematic tests of everyone in a facility are highly recommended if a few cases are identified, or one case without clear prior cause or existing quarantine. Cases happen in clusters and testing everyone can expose multiple presymptomatic or asymptomatic cases whose isolation will prevent a much larger outbreak.
Hygiene
- Increased cleaning and sanitizing of all high-frequency touchpoints at a pace compatible with the usage. These include door handles, elevator buttons, sinks, toilets, tabletops and frequently handled machinery, equipment, electronic devices and other items. Particular attention must be devoted to hand grips and stair rails.
- Checking and ensuring that soap dispensers and paper towels in bathrooms remain adequately supplied throughout the day.
- Providing hand sanitizers at all entrances, exits and high-traffic locations.
- Providing tissues and sterilizing alcohol-based wipes.
- Replace commercial-style open-ring dropdown toilet seats with those fully covering, and post signage encouraging closing before flushing (may reduce aerosolization of infection).
- Engineer door-opening and closing to minimize need for hand surface contact following hand-washing or use of restroom, or for the entrance to the buildings, or when crossing different sections of a building.
- Install electronic (IR) switches, or elbow-operated faucet handles or foot-operated sink controls to minimize need for hand surface contact following hand-washing. Provide signage instructing in use.
- Use paper towels for hand drying. DO NOT use air blower hand dryers as they are known to widely spread viral particles.

Dining and other High Contact Activities
- Shared dining facilities are high risk activities for transmission. A shift to separated in-room dining should be done in high risk areas.
- Where residents are sufficiently autonomous, provide in-room food service with no-contact prepared food delivery.
- Sanitize areas of contact after each individual use, including tabletop, chair armrest, menu. Use washable or disposable tablecloths and menus.
- Give support and tools (hand sanitizers or else) for hand hygiene before eating.
- Wait and service staff should avoid contact and proximity.
- Stagger dining times to avoid crowding and sitting arrangements to avoid face-to-face dining.
- Where contact is essential for services provided, careful handling protocols should be made including effective ventilation, gloves, disposable overgarments, and masks.
Employees and Corporate Environment
Staff and family members
- Educate staff and their families, as well as residents and their families, about coronavirus transmission and prevention. Ensure employees know that when they have even mild symptoms they should not be at work locations or in-person meetings and they will be paid and not penalized for sick days. Set up a reporting system for any cases (see Appendix A for a suggested “Employee Safety and Screening Questions for Employers”).
- Ensure employees have appropriate health insurance policies so that they will not be afraid to seek out care when they have symptoms, even mild ones.
- Ensure a proper and continuous supply of PPE for the workforce (see Appendix B for more info on PPE). Document proactive contingency plans for temporary PPE supply-chain interruptions. Eye protection (face shields or goggles) is to be encouraged along with masks or other face coverings (not as a substitute for masks). As a supplementary preventive measure, consider making masks or other face coverings available for workers’ families and household members.

Organizational considerations
- Prepare for employee substitutions in case they become ill individually or collectively.
- Implement proactive staff shortage contingency planning, possible use of trained staff augmentees
- Stay abreast of current information and advisories.
- Replace in-person office meetings with virtual ones.
- Implement staff buddy-care or other programs as appropriate to monitor for fatigue and precaution-measures burnout.
- Put in place redundant/resilient staff emergency contact procedures.
Decision-making processes
- Designate leadership/decision-making authority chain allowing for after-hours and disruptive events such as short-notice need for isolating multiple residents.
- Increase emphasis on / allocation of resources for ongoing short-format staff trainings – “in-services”, to stay current with evolving best practices for all staff.
- Designate Infection Prevention and Control Officer.
- Communicate with US HHS HealthCare Coalition Preparedness representatives or national equivalent.
Contingency planning
- Proactive contingency planning for community members (resident, new admission, visitor, vendor or staff) positive COVID notifications, and for the possibility of a superspreader event within the community, causing staff outages.
- Guidance for, and as feasible, minimizing population mixing with, outside providers of services–barbers, beauticians, podiatrists, other consultants and ancillary service providers.
- Request all symptoms and keep a record of them for community members and outside providers. In case they live with other people, also request their symptoms (they may be asymptomatic but the people living with them could be symptomatic).
- Request all travel information for community members and outside providers including cities to which they travel to find out if they are more at risk of contagion.
- Consult for community members and outside providers to determine if they are with infected people in their jobs (doctors, nurses…).
Air Quality
- Bring lots of fresh air inside:
- Minimize recirculation of stale air. When possible, keep ventilation and furnace fans ON to bring in outside air.
- Change air with fresh, clean air at least six-twelve times/hour (6-12 ACH) in workplaces, schools, gyms, other places people gather. Maximize in homes as possible.
- Open windows if they can really add fresh air.
- Evaluate and improve ventilation:
- Clean air with better filters (MERV-13 if possible).
- Supplement with portable HEPA-filter units, sized to the space. Avoid ionizers and ozone generation that are sometimes present in HEPA purifiers.
- Make DIY air cleaner (with MERV-13 filters or better and fan boxes) for homes, neighbors, community groups.
- Make sure that rooms are properly ventilated to ensure good air quality.
- Open windows.
- Determine air flow and circulation in rooms.
- Improve air flow if needed using supplementary mechanical ventilation such as fans, blowers, air exchangers and similar systems.
- If ventilation and fresh air intake is limited or impossible, use HEPA air purifiers.
- Incorporate HEPA filters and UV disinfection into air ducts of air conditioning systems.


Records
- Participate in national reporting, e.g. US Centers for Disease Control and Prevention National Healthcare Safety Network – Long-term Care Facility Module (CDC NHSN LTCF) or other nation equivalent.
- Record case lists – tabular record of residents with potential COVID symptoms and actual cases.
- Track and identify trends in weekly totals of acute care transitions – upticks have shown to be an early independent indicator of a possible outbreak.
Enhanced rule for areas active transmission
It is essential that High-Risk institutions follow Safe Zone practices and remain disease-free. When COVID-19 is found in a nursing home, the confirmed case and suspected cases (if any) should be immediately isolated from others and from each other (confirmed from suspected cases, and multiple suspected cases must be isolated from each other in case one of them is infected and the others are not, multiple confirmed cases may be isolated together). Off-site isolation should be facilitated when possible. Before entering the isolation area, cases should change their clothes and/or put on proper PPE such as gown, mask, face shield, gloves, etc. (see APPENDIX B for details on PPE and APPENDIX C for case definitions). Health care workers should adopt proper personal protection measures. Unnecessary personnel should be forbidden in isolation areas. Strict disinfection should be carried out for isolation areas and contaminated objects. (see APPENDIX D for more information on Isolation of confirmed, suspected or symptomatic residents)
Visitors
- If at all possible, avoid outside contact and encourage the use of text, phone and videoconference to communicate. Where visitors are necessary, consider setting up a separate area for visitor meetings, including enough space for everyone to remain at a safe distance (well over 6 ft), video links for virtual contact and glass or plexiglass partitions. Note: a necessary visit is defined as essential to maintaining mental and physical health, or is required in specific situations including end-of-life, change in health status or other pressing circumstances (e.g. financial or legal matters, family crisis).
- As soon as there are signs of an outbreak, the facility must provide masks (if possible N95) and they may be required even before outbreak confirmation.
- Deliveries should be made by single drivers who do not have symptoms of the disease and have not recently (within 14-21 days) had known exposures.
- Whenever possible, no-contact deliveries should be dropped off in a space that does not require entry into the facility.
- It is highly advisable that people allowed entrance into a high-risk institutional environment have been recently tested with negative results.
- Have a designated area for visiting; that area would be used only for necessary visits, as previously defined. Ideally this area should have direct access (not pass by various parts of the facility) & should be cleaned & ventilated as often as possible (ideally after each visit).
Testing
- Systematic and specific testing: If possible, DNA tests, qRT-PCR tests or possibly viral RNA tests or even the use of regular screening with pulse-ox meters where possible or other specific tests, should be applied widely and regularly (e.g. weekly, or every X days, etc.) to the workforce to identify and isolate individuals who are infected. This way of testing focuses on a specific facility or area, in order to identify potential cases to be isolated. If the test is specific enough and can be applied widely enough, this approach can stop an outbreak.
- CAUTION: COVID RT-PCR tests have a sampling induced false negative rates. Multiple tests are often needed to confirm a diagnosis. The false negative rates of RT-PCR may give false confidence to individuals who are sick to continue normal activities. Symptomatic individuals should not be considered to be COVID free even if they have negative test results. Therefore, RT-PCR tests cannot be relied upon by themselves for transmission prevention. Resolution of symptoms and multiple negative tests are necessary.
- Where RT-PCR test results are delayed, or for members of high risk institutions, or where isolation or workforce decisions must be made, CT-scans with lower false negative rates are better suited to ruling out a COVID diagnosis.
- Where persistent widespread testing within institutions is not possible due to resources or costs, pool testing can be used. Pool testing may be exploited in an optimal strategy, as an alternative to alleviate test availability or other limitations while still giving relevant information and controls. Since pool testing has its own issues with respect to false positive v. false negative rate, it should be used as a preliminary measure that is upgraded as soon as is feasible.
- Typically, the most important difficulty is false-negatives because of the initial self-reporting: people who are sick, but do not recognize it and don’t self-report, perhaps because symptoms are generic/nonspecific, or immediately life-threatening, or because of false negative test results. Asymptomatics also represent a major risk factor in care homes. Alternatively, individuals may suspect they have the disease but for personal, financial, social or professional reasons don’t choose to be diagnosed, or are not provided with the opportunity to be diagnosed, and isolated. Systematic testing minimizes the risk of both mildly symptomatic and asymptomatic being missed in the process and removes many social and professional reasons to avoid testing.
- Where effective contact tracing is operational, high-risk asymptomatic persons can be directed to present for testing, quarantined, or at a minimum explicitly discouraged or barred from visiting or working in the facility depending on local jurisdictions.
Employees, facilities and corporate environment
- Emphasize to employees that their actions outside of work can lead to transmission of infection risking the lives of residents. Education should include how to mitigate risk to their families and households as well as to residents of the facilities where they work. Even if the disease has a low risk to them, any contact with individuals or surfaces in non-safe areas is extremely dangerous for those in the high-risk facility. They should take responsibility and limit off-work non-safe contact to a minimum, while their employers/facilities are making face coverings and/or masks available to their close relatives.
- Encourage employee adoption of safe space protocols at home limiting their contact and others who live with them with individuals and surfaces that are not safe and record which employees are following them on a voluntary basis. Note: a “Safe space” is defined by the CDC as a space where people can self-isolate or practice social (physical) distancing between themselves and other people who are not from the household.
- Encourage employers and facilities to communicate with workers and supervisors in order to prioritize and plan as soon as possible to: ○ pay workers enough so they don’t need multiple jobs to subsist. ○ give workers enough hours so that they can work in only one place, and get good health insurance for themselves and their families. ○ find appropriate staffing levels for each type of worker so that there are the minimum number of staff coming in and out, and at the same time preventing overwork, exhaustion, burn out.
- Ensure additional and greater supplies of PPE equipment for the workforce (see Appendix B for more info on PPE). As a supplementary measure, ensure masks or face coverings are available for workers’ families.
- Engage with local medical facilities/laboratories or local and state/provincial public health agencies, to coordinate rapid testing and contact tracing of residents and employees.
- Partition facilities to separate zones, limiting employees and residents from crossing from one zone to another. This will limit contagion, in case one zone becomes infected.
- Stagger breaks and discourage socializing within indoor confined areas. Ensure mask wearing even for staff-staff interactions and ensure proper training in PPE wearing/fitting.
- Transfers of residents in or out of the institution should follow safe space requirements with attention to point of origin, point of destination, contact with those performing the transfer, and the vehicles that are involved. (see Appendix E for more informations on receiving residents being discharged from hospital)
- When bringing in new residents or starting new employees who are not coming from a Safe Zone quarantine for 14-21 days.
- Where possible, arrange facilities for residential accommodation of employees within this or another Safe Zone.
- Arrange partnerships with sister institutions to follow Safe Zone practices for transfers and response to an outbreak.
- Arrange for office staff to work from home, develop protocols so that this is possible (for example, see Appendix F for more information on decontamination and cleaning processes for care homes with possible or confirmed cases of COVID-19).
- Avoid clustering in elevators. Elevators should not take more than half of their carrying capacity.
- When AC is used, disable re-circulation of internal air. Clean/disinfect/replace key components and filters weekly.
- Check the engineering design of the ventilation system to determine if air flows connect air from different rooms. Develop mitigation or alternative ventilation processes.
- Deploy air purifiers using HEPA filters around the facility.
Key measures taken in some states and countries having success in protecting care homes residents
See [4] “European Observatory and Health System” for more details.
- Strengthening medical support
- Reducing and managing visitors to prevent infection
- Establishing long-term care COVID control task force
- Devising creative ways to enable visits with relatives
- Providing guidance – staff, residents, visitors, outside consulting and ancillary-service providers
- Minimising infection through workforce management
- Providing financial support to workforce and facility operators
- Boosting staffing levels recruitment and retention
- Repeat testing for staff
- Centralising procurement of equipment
- Planning for isolation and quarantine
- Expanding testing for residents
- Nursing Homes in COVID-19 time: Why so many examples of failure to care and protect? Last update for the #outreach-high-risk-institutions on the Nursing Home project on Medium: https://towardsdatascience.com/nursing-homes-in-covid-19-time-why-so-many-examples -of-failure-to-care-and-protect-e0ea38f6fd2c
- Adapted from Stephane Bilodeau, Briggs Clinco, Jeremy Rossman, Gary Chizever, Derrick Van Gennep, Andrew Zamora, Tracy Baving, Jonathan Tagliavini, Rachel Cohen Yeshurun, Katie Marsh, Leo PeBenito, Naomi Bar-Yam, Aaron Green, Yaneer Bar-Yam, COVID-19 Guidelines for High Risk Care Institutions, EndCoronavirus.org, July 31, 2020
- The Vivaldi study by the ONS: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/impactofcoronavirusincarehomesinenglandvivaldi/26mayto19june2020
- European Observatory and Health System study:https://analysis.covid19healthsystem.org/index.php/2020/06/08/what-measures-have-been-taken-to-protect-care-homes-during-the-covid-19-crisis/



