by Nathanael C. Nerode – 03/21/2023
“If you are somebody who runs a building, operates a building, it is incumbent on you to make sure that the place you run, the place you own, does not become a place that unnecessarily spreads viruses, gets people sick, fills up our hospitals, causes unnecessary suffering and death.”
— Ashish Jha, White House Covid-19 Response Coordinator,
at White House Summit on Indoor Air Quality
Hospitals and medical offices are infecting people with COVID. Routinely.
This is preventable. Easily; affordably.
- Portable plug-in HEPA filters ($100) in every exam room
- P100 elastomeric respirators (reusable for years, $37) on all medical staff
How to Stop COVID & Other Airborne Diseases
How COVID Spreads
- COVID is an airborne virus that hangs in the air like fog and spreads like smoke. [2]
- The virus enters the air as an aerosol [3] when any infectious person breathes out [4] – breathing is an aerosol-generating procedure. [5]
- The virus aerosols can remain in poorly ventilated rooms (e.g. medical exam rooms) for hours. [6]
- After one unmasked, infected person breathes out in a room, the aerosols in the room can infect patients, nurses, and doctors for hours, long after the infected person has left the building.
How to Stop COVID: P100 Respirators, HEPA Filters
Infection can be prevented by:
- removing the virus from the air using HEPA filters, or a similar MERV-13 or better filter with a high Clean Air Delivery Rate (CADR). Proven to work in a Cambridge, UK hospital. [7]
- circulating fresh air into the room, with a high enough CADR rate (but this has heating issues)
- an infected person wearing N95 or better PPE, with source control, to filter the virus before it gets into the air
- anuninfected person wearing N95 or better PPE to filter the virus out of the air before it reaches their mouth and nose. Shown to protect nurses in a Cambridge, UK hospital. [8]
When used properly:
- N95 respirators reduce viral load by 95% or more (FFP2 is equivalent, KF94, KN95 similar)
- N99 respirators reduce viral load by 99% or more (FFP3 is equivalent)
- P100 respirators, which are all reusable, reduce viral load by 99.97% or more (P3 is similar)
- HEPA filters reduce viral load by 99.97% or more, each time the air goes through the filter
Proper use means:
- respirator with source control is worn at all times indoors at work
- respirator fits tightly, no leaks around the edge (“elastomeric” silicone/rubber edges help)
- air filters are always turned on and operating
- air filters provide high enough CADR to clean the air in the room between patients / visitors
- ASHRAE standards [9] say CADR of 6 ACH (cleaning air every 10 minutes) is the bare minimum, but 12 ACH (cleaning air every 5 minutes) is more suitable, for healthcare settings
These are very affordable.
- A HEPA air purifier large enough for a small exam room costs less than $100 [10] retail
- A fully reusable P100 respirator costs less than $37 [11] retail. Filters ($6-$17) last over a year. [12]
- A list of P100 respirator options and more info: https://cleanaircrew.org/elastomeric-respirators
These provide visible evidence of precautions.
- Patients & staff, particularly those at high risk, need to know that they are in a safe environment.
- P100 elastomeric masks with source control provide visible evidence that the medical staff is protecting patients.
- Portable, plug-in HEPA filters provide visible evidence that the air is being cleaned between patients. (The patient cannot see whether the main building HVAC system is cleaning the air.)
Even with imperfect use, these methods can greatly reduce transmission.
Frequently Asked Questions on Safe Medical Offices: Respirator Masks
We’re testing our staff, do they still need respirator masks?
- Yes. A person can have a negative test in the morning and be infectious in the afternoon.
Our staff are vaccinated, do they still need respirator masks?
- Yes. Vaccinated people can be infected and can infect other people.
We have HEPA, do staff still need respirator masks?
- Yes. It takes at least 5 minutes for all the air in the room to go through the HEPA filters.
With two people in the same room, one can infect the other before the air has a chance to go through the HEPA filter. - Patients must remove their masks for medical exams of the nose and mouth. It is vital for the air around the patient to be safe and clean when they are unmasked.
Do the respirator masks need to be fit-tested?
- Even without formal fit-tests, respirators reduce risk massively. [13] Respirators should be issued and used immediately to reduce exposure, even before doing fit testing.
- Fit tests are highly desirable and improve effectiveness. The fit test kit only needs to be bought once for the entire office or hospital, or can be rented. If the certified fit test equipment is not required by regulation, a cheaper qualitative fit test is available from https://fittests4all.bigcartel.com/
What respirator masks should we issue? What respirator masks should we allow for staff?
- All masks for medical staff should be rated to filter at least 95% of viral particles and should have source control (so breath out is filtered as well as breath in).
- Most people find that reusable elastomeric (rubber-edged) masks are more comfortable than disposable masks. All P100 and P3 masks are elastomeric. They are more cost-effective in the long run than disposables, since they last for years and the filters only need to be replaced once a year.
- Different people find that different masks fit better. Individuals should be allowed to use alternative respirator masks as long as they meet one of the standards.
- The N95 standard was originally designed for males of European descent. [14] Many people find that they can get a better fit with American N99 or P100 standards, or foreign KF94, KN95, FFP2, FFP3, or P3 standards.
- A final option for staff who cannot find anything else which fits, or who have impaired breathing abilities and lack the lungpower to pull air through a respirator, is the Powered Air Purifying Respirator (PAPR). These are not as sensitive to fit.
What about “surgical”/”medical” and cloth masks?
- These only reduce viral load by 30%, [15] even worse if they fit loosely.
- They are better than nothing, and it does reduce exposure risk some if patients wear them.
- Normally, these should NOT be used by medical or surgical staff, who should use N95 or better.
But I thought there was a study saying that masks didn’t work?
- Every valid study shows that respirator masks (N95, N99, P100, FFP3, P3), used consistently, work.
- A few controversial studies, where people would take their masks off half the time, have been publicized in a way which confuses people. Masks, unsurprisingly, only work if you wear them.
- Some studies were of “surgical”/”medical” masks, which are not very effective (see above).
Frequently Asked Questions on Safe Medical Offices: Air Filters
If we have respirator masks (N95, P100), do we still need HEPA in every room?
- Yes. Patients must remove their masks for medical exams of the nose and mouth. It is vital for the air around the patient to be safe and clean when they are unmasked.
- One asymptomatic patient can infect the air in the room. The air must be cleaned before the next patient takes their mask off in the same room.
How do I know whether I have powerful enough HEPA filters?
- Air filters have a CADR (Clean Air Delivery Rate) measured in CFM (cubic feet per minute).
- Calculate the cubic feet in a room by measuring the room (length, width, height).
- Divide this by the CFM rating to see how many minutes it takes to replace the air in the room.
- Replacing the air every 5 minutes is 12 “air changes per hour” (ACH).
- Because of uneven airflow, you want a margin of safety: in practice it may take twice as long for air in some corners of the room to be replaced.
- Experimental studies show that replacing the air by clean air every 5 minutes (i.e. 12 ACH) is necessary to provide the same protection from far-field exposure as an N95 mask. [16]
- This is needed to assure the patient that it is safe to remove their own mask for a medical exam.
- The more frequently the air is cleaned, the better the risk reduction. Higher ACH is better.
What about fresh air?
- Fresh air from outdoors can provide clean air just like HEPA filters, and has other benefits.
- Fresh air must be heated or cooled, adding expense. It is hard to get enough fresh air indoors.
- CO2 concentrations above 800 ppm indicate that there is not enough fresh outdoor air to remove the virus. According to the EPA, “If unable to get below 800 ppm, increased reliance on enhanced air filtration (including portable air cleaners) will be necessary.” [17]
What about upgrading the main building HVAC?
- Main building HVAC can be upgraded with better filters to provide CADR similar to putting portable HEPA filters in every room.
- However, it is impossible for patients, doctors, or nurses to personally check whether the main building HVAC is performing as advertised. Many HVAC systems stop operating properly, stop providing enough clean air to one or two rooms, and people don’t notice for weeks.
- Upgrading the primary building ventilation system to have suitable air filtration can take years.
- If this approach is taken, you need a third-party certification for every room by an air quality engineering expert. This certification must be published and posted so patients know they are safe.
- Putting portable HEPA filters into each hospital room, exam room, waiting room, and restroom can be implemented within weeks, and verifying the air change rate is easy.
What about UV disinfection?
- UV disinfection can be used to remove virus from air.
- UV is difficult to engineer correctly and requires a consultation from a specialist to use correctly.
- HEPA can be installed immediately and are typically cheaper.
What about ionization, “foggers”, and other “secret sauce” systems?
- These do not work for stopping viruses, and are often harmful.
- Any system which puts chemicals in the air or generates new chemicals in the air, including ionization, should be avoided according to ASHRAE. [18]
Frequently Asked Questions on Safe Medical Offices: General
Do respirator masks and air filters help prevent other diseases in addition to COVID?
- Yes. Influenza [19] is also airborne by aerosols. Strep A is also airborne by aerosols. So are many other diseases, particularly respiratory infections.
- Respirator masks (N95, P100) protect against all these diseases at once.
- HEPA filters remove all these diseases from the air.
Will these precautions mean our staff is healthier and will take fewer sick days?
- Yes. Respiratory illnesses probably account for 50%-70% of all absences from work. [20]
- Roughly 30% of these illnesses are probably caught at work. [21]
- The same precautions (respirator masks, air filters) protect against all respiratory infections.
How likely is it that we’ll infect people with COVID if we don’t take these safety measures?
- Very likely. COVID is in “high community transmission” throughout the US. It is very likely that any person walking in the door has COVID, possibly asymptomatic. All inpatient areas are high risk.
- CDC [22] recommends N95 or better masks when encountering patients with known or suspected COVID.
- ASHRAE standards [23] for health care recommend that high-risk inpatient areas have at least 12 ACH.
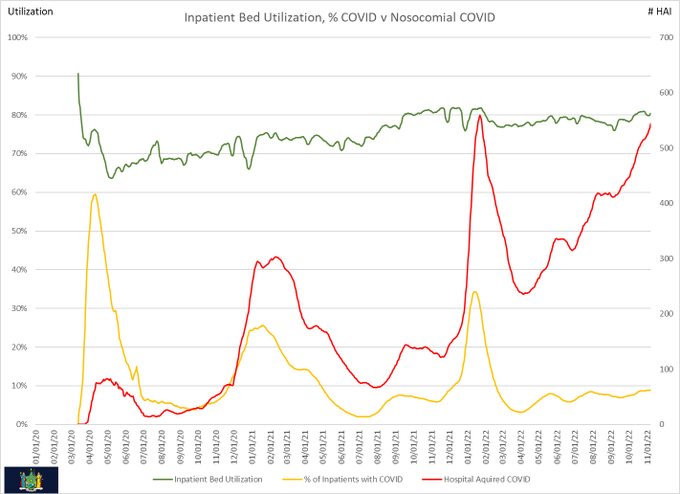
- There are currently numerous proven hospital-acquired cases of COVID.
How likely is it that a random patient has COVID? I thought rates of COVID weren’t high?
- No. As of February 2023, the CDC community transmission map shows “substantial” or “high” transmission throughout most of the US. [24]
- The CDC has also released a misleading and confusing “community levels map” which instead shows whether the hospitals are overloaded; [25] some people may have been confused by this.
Why didn’t our office already receive an announcement about this from CDC or WHO?
- Good question. [26]
- Much of the medical profession only learned the scientific consensus that COVID is spread by aerosols in late 2020. [27]
- CDC & WHO have updated their technical guidance to recommend respirators [28] and HEPA. [29]
- However, there is currently no WHO or CDC publicity campaign corresponding to the new guidance.
Where can I get more information?
- The World Health Network has a clearinghouse of information and is in constant communication with the top scientific experts. https://worldhealthnetwork.global/
- Clean Air Stars maintains a database of plug-in HEPA and similar air filters, with airflow ratings (CADR), noise ratings, and prices. https://cleanairstars.com/
- Clean Air Crew has a list of elastomeric respirators, and links to NIOSH-approved list of respirators with source control. https://cleanaircrew.org/elastomeric-respirators/
Respirator masks look intimidating to some people. Can we make them look cool?
- Reusable elastomeric masks, such as P100 masks, are mostly made of hard plastic.
- The hard plastic parts can be decorated safely, with stickers or paint, without impacting effectiveness.
- For some examples, see https://masksquad.bigcartel.com/ and http://masksquad.com/
- Companies (e.g. Optrel, OmniMask) are developing respirators with transparent face windows for use with people who read lips.
References
1 Visualization by Michael Olesen at https://icemsg.org/graphs/new-york/ (click on Util-HAI at the bottom). Data from https://healthdata.gov/Hospital/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/anag-cw7u “The following dataset provides facility-level data for hospital utilization aggregated on a weekly basis (Friday to Thursday)”
2 https://time.com/5883081/covid-19-transmitted-aerosols/ Time Magazine/ “COVID-19 is Transmitted Through Aerosols. We Need to Adapt.” Professor Jose-Luis Jimenez, University of Colorado-Boulder, Fellow of the American Association for Aerosol Research. One of many scientific papers on this topic is https://www.medscape.com/viewarticle/934837 “Arguments against aerosol transmission don’t hold water”, by Jimenez.
3 “Small particles (also known as aerosols) are released when a person breathes, talks or vocalizes, sings, coughs, or sneezes. These small particles can remain suspended in the air for a period of time and can move beyond six feet on air currents. Other people might inhale these small particles even if they are farther than six feet away. Inhalation of airborne particles suspended in the air is now considered the primary route of transmission for COVID-19 infection.” From Cal/OSHA Interim Guidance for Ventilation, Filtration, and Air Quality in Indoor Environments, February 23, 2023 https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Interim-Guidance-for-Ventilation-Filtration-and-Air-Quality-in-Indoor-Environments.aspx
4 https://www.ijidonline.com/article/S1201-9712(22)00589-6/fulltext International Journal of Infectious Diseases: “Viable SARS-CoV-2 detected in the air of hospital rooms of COVID-19 patients with early infection” Kitagawa et al.
https://www.pnas.org/doi/10.1073/pnas.2006874117 “The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission”, Stadnytski et al. Many more references on request.
5 https://jamanetwork.com/journals/jamasurgery/fullarticle/2774161 JAMA (Journal of the American Medical Association) Surgery. “What is An Aerosol Generating Procedure?” Klompas, Baker, Rhee.
6 “SARS-CoV-2 remained viable in aerosols throughout the duration of our experiment (3 hours)”, https://www.nejm.org/doi/full/10.1056/NEJMc2004973 “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1”:
7 https://pubmed.ncbi.nlm.nih.gov/34718446/ “The Removal of Airborne Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Other Microbial Bioaerosols by Air Filtration on Coronavirus Disease 2019 (COVID-19) Surge Units” Andrew Conway Morris, et al.
BBC news report regarding this study is at https://www.bbc.com/news/av/uk-england-cambridgeshire-59490424 “Cambridge doctors gobsmacked by air filter’s effect on COVID”.
In this study, samples were taken directly from the air. Without HEPA filters there were many pathogens in the samples. With HEPA filters, almost none.
8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8635983/ “Efficacy of FFP3 respirators for prevention of SARS-CoV-2 infection in healthcare workers”, Mark Ferris, Rebecca Ferris, Chris Workman, et al. FFP3 is the European equivalent of N99, filtering 99% of particles.
9 ASHRAE Standard 170-2021 for ventilation of healthcare facilities.
10 Levoit Core 300 has a high enough Clean Air Delivery Rate for a small medical exam room, and was selling for $89 on Amazon on 12 February 2023, with a list price of $100.
11 The 3M 6100 (small), 6200 (medium), and 6300 (large), the base respirator mask, were selling for less than $10 each on Amazon on 12 February 2023, with list price $21. The P100 filters for it (#2091) come separately; you need two per mask. The filters cost $18 for a pack of 6 filters (for three masks), which is $6 per mask. This particular respirator requires an add-on filter for source control, the #604 exhalation valve filter, which is only sold in packs of 6 (you need one per mask), for $55 at time of writing ($9.18 per mask). $21 + $6 + $9.18 < $37.
GVS Elipse With Source Control (available in two sizes) was selling for $28 on Amazon on 12 February 2023, including P100 filters. A pair of replacement P100 filters for this respirator (2 filters per mask) costs $17.
12 The Texas Center for Infectious Disease has been using a Honeywell P100 design for years. Every test with these masks shows that the filters last at least a year.
https://elemental.medium.com/a-tiny-hospital-in-texas-might-help-solve-the-mask-shortage-9ad3c0a7a861
13 https://doi.org/10.1080/15459624.2010.514782 “Fit testing respirators for public health medical emergencies”, Journal of Occupational and Environmental Hygeine, Lisa M. Brosseau, 2010; subjects with no training got fit levels of 10, much better than is achievable with any “surgical” or cloth mask.
https://pubmed.ncbi.nlm.nih.gov/21477136/ “A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers”, MacIntyre et al., 2011., pre-pandemic “Rates of infection in the medical mask group were double that in the N95 group.” “There was no significant difference in outcomes between the N95 arms with and without fit testing.” “
14 https://www1.racgp.org.au/newsgp/clinical/many-n95-respirators-do-not-properly-fit-women-or “Many N95 masks do not properly fit women or people of Asian descent”
15 https://www.nature.com/articles/s41370-021-00337-1 “Assessing the effect of beard hair lengths on face masks used as personal protective equipment during the COVID-19 pandemic”, Journal of Exposure Science & Environmental Epidemiology, Prince et. al. The graphs are very informative. “The FFE percentages for a reusable cloth mask (D) and a procedure mask with elastic ear loops (E) were low even with shaven skin”.
16 https://www.medrxiv.org/content/10.1101/2022.08.09.22278555v7.full.pdf “What ACH is equivalent to an N95 for protection from SARS-CoV-2 and other airborne contaminants?” Devabhaktuni Srikrishna.
17 https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html EPA: “COVID-19: Ventilation In Buildings”
18 https://twitter.com/WBahnfleth/status/1504543122075922437
“The only air disinfection technology that ASHRAE identifies as being effective and safe is germicidal UV. That has been in its Airborne Infectious Diseases /Infectious Aerosols position document since 2009. The current state of knowledge about a log of other air cleaners is that they may not work and may have safety issues. That’s why they aren’t recommended. ” Bill Bahnfleth, Chair, ASHRAE Epidemic Task Force, March 17, 2022.
19 https://docs.google.com/document/d/e/2PACX-1vTnR8CNo_Q-ohy8EJ0NkfG3TGcC-1YFBxWil1HsjK6JLYwbDkWphcHCbN4A6ReVBVL01nBCEGwl4i_e/pub has a long catalog of citations for various illnesses being airborne by aerosols, including COVID and influenza
20 https://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-1-3 “A study of indoor carbon dioxide levels and sick leave among office workers “, quoting other studies: “In a study conducted by Nichol et al., upper respiratory infections accounted for approximately 65% of sick leave days among working adults [11]. In a study of military aircrews, respiratory infections accounted for 70% of the total number of days the crews were grounded [12]. In a study conducted on government employees in the United Kingdom, respiratory infections and gastroenteritis accounted for over half of all absences [13]”.
https://www.bls.gov/opub/ted/2022/7-8-million-workers-had-an-illness-related-work-absence-in-january-2022.htm “The number of workers who are absent because they have an illness, injury, or medical problem or appointment regularly spikes from December through March, coinciding with the peak in cold and flu seasons…. The increase in absences during January 2022 partly reflects the increase in COVID-19 cases, along with seasonal illnesses.” Article from TED: The Economics Daily, Bureau of Labor Statistics, US federal government, February 9. 2022
21 Ibid. “In a study first published in 1960, Gwaltney and his colleagues conducted an extensive study at a large insurance company. Their results suggested that working adults were responsible for introducing 32% of the colds their families contracted [5–7].”
22 https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html “HCP who enter the room of a patient with suspected or confirmed SARS-CoV-2 infection should adhere to Standard Precautions and use a NIOSH-approved particulate respirator with N95 filters or higher”
23 ASHRAE Standard 170-2021 for ventilation of healthcare facilities.
24 This is the direct link to the actual community transmission map:
https://covid.cdc.gov/covid-data-tracker/#county-view?list_select_state=all_states&data-type=Risk
25 “The new framework [“community level” map] instead focuses on the situation in hospitals — how many people are being admitted for COVID-19 and how much capacity is left…. Experts in public health and infectious disease NPR interviewed say that for the average American trying to decide on behaviors like going to restaurants, the CDC’s new blueprint for navigating the pandemic leave them with an incomplete picture of their individual risk.”
https://www.npr.org/sections/health-shots/2022/03/10/1085797307/cdcs-new-covid-metrics-can-leave-individuals-struggling-to-understand-their-risk “What’s the COVID risk in your area? CDC maps leave some people confused”. National Public Radio, March 12, 2022.
26 https://thetyee.ca/Analysis/2022/12/21/Ten-Downplayed-COVID-Facts/
27 https://www.wired.com/story/the-teeny-tiny-scientific-screwup-that-helped-covid-kill/ “The 60-year-old Scientific Screwup That Helped COVID Kill”, Megan Molteni, WIRED Magazine, May 13, 2021
28 CDC: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/use-n95-respirator.html ;
WHO: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-masks
29 CDC: https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html#refphf
WHO: https://www.who.int/publications/i/item/9789240021280











