A Comprehensive Beginners Guide to the Ongoing COVID-19 Pandemic (UK Edition) … or Why and How to Minimise Reinfection
Is the ongoing debate on COVID-19 a conspiracy theory?
No, it isn’t. Everything explained here is supported by peer-reviewed scientific research published in reputable journals. The problem is that UK government and public health policy has diverged from the science in favour of short-term economic gains. However, this is not a sustainable solution.
Sources are provided for every single claim made here so they can easily be verified.
But hasn’t COVID gone away?
Not at all. COVID-19 continues to spread, and each infection carries the risk of Long COVID, which can cause lasting organ damage, cognitive impairment, and chronic illness1.
In absence of valid and accurate official data, there are clues suggesting that there are still many people being infected with COVID:
- The World Health Organisation still considers COVID a pandemic, it has simply ended the emergency phase2,3.
- The Winter Coronavirus Infection Survey estimated that at the end of December 2023, around 1 in 24 people were infected with COVID*4.
- The ZOE COVID Study, a private study which ran until September 2023, showed that even during times of the lowest transmission, approximately 500,000 people in the UK were infected at any one time11. The current UK population is around 67 million people5.
- Other countries continue to collect wastewater data and show repeated peaks of infection in all seasons throughout the year- including Scotland, the Netherlands, the USA and Canada6,7,8,9.
- In 2022, more people were hospitalised with COVID in the UK than in 2020 or 2021. Due to significantly reduced testing, numbers for 2023 are unreliable; however, lack of any mitigations means it is likely the true figure for 2023 is similarly high10.
Official case numbers can appear low due to the following:
- Testing is no longer encouraged11.
- Free tests are not available to the majority of the population11.
- There is no way to report positive results from privately purchased tests11.
- Hospitals no longer routinely screen for COVID, even in symptomatic patients12.
- Lateral flow tests have a high false negative rate compared to PCR tests, meaning a lot of infections are not detected. This is further exacerbated by not swabbing the throat and only testing on the first day of symptoms, given viral load peaks between days 3–413-16.
- In England, Wales and Northern Ireland, wastewater is no longer monitored for COVID to check for disease prevalence17,18,19.
Limitations with official case numbers make it difficult to know exactly how many infections are happening. Other factors contributing to the appearance that COVID-19 is no longer a problem include:
- Excess death data now includes the years 2020–2023 to generate the baseline number of expected deaths, therefore meaning that far more deaths are expected each year than before the pandemic. This hides the true number of excess deaths.22,23.
Don’t previous infections and the vaccine make me immune to COVID?
Sadly, no. Previous infections and vaccination provide some protection (“immunity”) against hospitalisation and death, but immunity against infection can wane rapidly24.
Studies show:
- Any immune protection against reinfection wanes rapidly after the initial infection. Reinfections are common and there are records of it happening in as little as 16 days25,26
- New variants evade prior immunity from vaccinations and infection27,28.
- Vaccines provide limited protection against infection and effects wane rapidly, this is compounded by fewer and fewer people being offered booster doses29.
- Herd immunity with COVID-19 is not possible30,31.
But isn’t COVID mild now anyway?
No. COVID has often wrongly been compared to the common cold or flu but is much more than a simple respiratory illness. SARS-CoV-2, the virus that causes COVID, is a virus which simply uses the respiratory tract to enter the bloodstream where it causes systemic inflammation and attacks blood vessels throughout the body32.
The disease that SARS-CoV-2 causes can be divided into acute and chronic phases. Vaccines mean that the acute phase can seem milder in most people; however, they provide limited protection from chronic illness and organ damage33,34.
As we learn more about the chronic phase, SARS-CoV-2 appears more similar to HIV, Epstein-Barr virus, syphilis, herpes and hepatitis B and C, illnesses which may cause initial flu-like symptoms but for which most concern lies in their long-term harm. Both the acute and chronic phases of COVID can be symptomatic or asymptomatic, but lack of symptoms does not mean there is a lack of internal damage.
Studies show that COVID infection:
- Results in ongoing symptoms in at least 10-20% of infections, which can be disabling35,36.
- Increases risk of cardiovascular illness for at least a year following mild infection, resulting in increased blood clots, heart attacks, strokes and pulmonary embolisms37,38,39.
- Increases heart attack risk by 3–8x40 (in comparison, smoking increases heart attack risk by 2–4x yet indoor smoking is banned41).
- Leads to reduced global brain size and grey matter loss in 100% of patients with mild illness, compared with controls, as shown by MRI42.
- Causes cognitive impairment and reduced IQ compared to non-infected individuals —including 2–3x more cognitive impairment in healthcare workers following infection—with potential implications for healthcare delivery43,44,45.
- Increases risk of many autoimmune diseases, with one study finding an overall increased risk of 43%46,47.
- Increases risk of newly acquired Alzheimer’s and Parkinson’s diseases and accelerates existing disease48-53.
- Causes autonomic nervous system dysfunction54-58.
- Causes reduced sperm count, decreased sperm motility and increased risk of erectile dysfunction59-69.
- Causes immune dysfunction, including reduction in T, B, NK and dendritic cells70-81.
- Is associated with increased severity of RSV and Group A Strep infections both during COVID-19 infection and for at least one year post infection82,83,84.
- Induces gene expression associated with cancer formation and may be accelerating existing cancers85-91.
- Occurring initially during pregnancy results in twice the risk of a neurodevelopmental diagnosis at 1 year, as well as reduced lung volume and potential intestinal inflammation in baby92,93,94.
- Occurring initially during pregnancy causes an increased risk of miscarriage, pre-term and stillbirth as well as increased maternal morbidity and mortality95-99.
- In infants results in significantly poorer psychomotor development and higher rates of mildly delayed performances at 18–24 months100.
- Results in subclinical heart and lung damage in children who have seemingly recovered101,102.
- Results in increased risks of epilepsy, encephalitis, and nerve disorders in children for at least 2 years after infection103.
- Accelerates biological ageing on a cellular level104.
- Can result in viral persistence for months and, in some cases, years after initial infection even in patients without Long COVID symptoms such as fatigue, breathlessness and cognitive deficits. Persistent virus has been found in the brain, penis, testes, eyes, breast, appendix, gut, and muscle tissue105-112.
The possibility of chronic illness from SARS-CoV-2 was not unpredictable, as many infected with SARS-CoV-1 during the SARS epidemic of 2003 continue to have ongoing impacts many years later113,114. Studies show that risks of long covid symptoms and multisystemic damage are cumulative with each infection115,119.
The number of papers showing the long-term risks of COVID infections continues to increase into 2025, and it is becoming increasingly apparent that repeated infections are unsustainable and incompatible with a healthy, long life.
Surely if all this was happening, I would see it around me?
There are frequent reports and news articles showing the effects of the ongoing pandemic, but many fail to mention COVID as a major cause of what they report, or make unsubstantiated claims about other causes, such as lockdowns. In some cases, data is only available from countries outside the UK, but as COVID has spread globally, it is likely that the same is happening in the UK but without being documented or reported on.
- Since 2021, UK news outlets have been reporting people experiencing “brutal” and “super” cold symptoms, with prolonged illness and back-to-back infections120-123. This correlates with COVID-induced immune dysfunction, though this explanation is rarely given.
- Incidence of infections most commonly seen in immunosuppressed people has increased since 2020- including increases in Tuberculosis, Shingles and the invasive fungal infection Candida auris124-131.
- Excess deaths from heart attacks are ongoing, with the greatest excess in 25–44-year-olds, estimated at 23–34% excess deaths in this age range (for every 100 people expected to die from a heart attack, 123–134 are actually dying)132.
- UK insurance companies report a sudden rise in life insurance claims for people in their 40s133.
- In Germany a news source reports that record sickness rates last year caused a recession when the economy would otherwise have grown134.
- The Health Foundation reports that there is an upward trajectory of people not working due to ill health in the UK which is causing significant economic consequences135.
- The number of people on long term sick leave in the UK has hit a 30-year high136.
- NHS waiting lists have hit a record high136.
- Hospital trusts across the country are repeatedly declaring critical incidents due to significant and sustained pressures137-140.
- Schools are seeing consistently higher rates of chronic absenteeism than before 2020 in the UK and US141,142,143.
- A news article by Infection Control Today suggests that recent marked increases in violent crime and aggression in the US and Canada may be attributable to COVID-induced brain damage144.
- Record numbers of performers are cancelling shows and tours due to serious illness–COVID itself is rarely named as the cause as show cancellation policies usually exclude COVID-related cancellations145-150.
- A report from Singapore’s Minister for Health states that all “non-COVID” excess deaths could be linked to prior COVID infection, according to a new study in the country151,152.
- A Spanish university found that students infected with COVID were nearly half as likely to achieve outstanding academic results compared to their uninfected peers153.
- Doctors are reporting on social media that they are seeing increasing numbers of cardiac issues, strokes, blood clotting issues, new autoimmune disease, and psychiatric symptoms after COVID infections154,155.
- There has been a significant rise in children and teens diagnosed with type 1 diabetes, an autoimmune disease, since the pandemic began. One recent study found COVID infection results in 6x the risk of type 1 diabetes in children156,157,158.
- When last reported in March 2024, there were 2 million people reporting Long COVID symptoms in the UK, including 111,000 children159. This is nearly double the 62,000 children reporting Long COVID symptoms in March 2023160.
What about immunity debt?
Immunity debt is the misguided concept that due to COVID precautions reducing numbers of other common infections in 2020 and 2021, people are now becoming ill more often and more severely as they catch them again161,162. “Immunity debt” is not an established phrase used in epidemiology and was first used only in 2021163.
It is true that lack of exposure could lead to greater numbers of infections, as three years’ worth of newly susceptible people (babies and the newly frail/immunocompromised) would all become exposed to common illnesses in 2022. However, this would not lead to more severe or prolonged infections161,162. Epidemiologists and immunologists instead attribute this to COVID weakening our immune systems162.
There is no evidence to suggest that delaying infections results in more severe infection. In very young children, it can even be beneficial to delay infection until their immune system is fully developed. The immune system is not a muscle and does not need to be used constantly to be kept in shape. If anything, frequent infections can lead to malfunction161,162,163.
If immunity debt existed:
- A debt would also have been created by cleaning the water, developing sewers, and handwashing.
- People who go to space, or live on bases in the arctic, would develop an immunity debt from being isolated for years at a time.
- Children born after 2021, when lockdowns ceased, would not also be experiencing more severe and prolonged illness symptoms.
- The debt would have been paid in 2022, yet in 2023 severe and prolonged viral illness symptoms continue to affect the population.
I always wash my hands, won’t that protect me?
No, COVID is predominantly airborne.
- COVID is exhaled with normal breathing and talking and moves through the air like secondhand smoke164,165,166.
- COVID can linger in poorly ventilated rooms for hours after an infected person has left164,165.
- The majority of infections are from inhalation of the virus164,165,166.
- Despite hand washing being important to reduce transmission of some other illnesses, there is no evidence to show that handwashing significantly reduces transmission of airborne diseases such as COVID167.
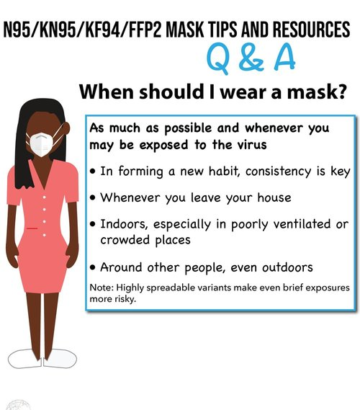
Do masks work?
Yes. Studies show that masks are effective in reducing the transmission on COVID-19, both on an individual level and in the community as a whole. However, not all masks provide the same level of protection. Whilst cloth and surgical masks do somewhat reduce transmission, respirator masks are far more effective 176-179.
But if masks really work, why aren’t they still in hospitals?
Once again, the removal of COVID protections in hospitals comes despite calls from healthcare workers, healthcare charities, scientists, and clinically vulnerable patients for them to remain180-187. There is an abundance of evidence to show masks reduce transmission176,177.
In the UK most hospitals have completely removed mask mandates, as well as stopping regular staff testing and permitting staff to return to work after infection without a negative test. This is despite the persistent World Health Organisation guidance that:
- [You should] wear a properly fitted mask when physical distancing is not possible and in poorly ventilated settings188.
- [You should] stay home and self-isolate for ten days from symptom onset, plus three days after symptoms cease188.
- If you need to leave your house or have someone near you, wear a properly fitted mask to avoid infecting others188.
- Universal masking should be used in healthcare facilities where there is community transmission of COVID189,190,191.
Occasionally, during significant and sustained pressures, temporary mask mandates do return in some hospital areas, indicating an understanding that these do reduce infection. However, this limited action does little to protect against year-round infections. It would be unthinkable to only mandate healthcare workers to wash hands during surges in norovirus or MRSA – why are mask mandates any different?
Data and studies show that current lack of COVID protections in healthcare is causing avoidable harm:
- At least 14,000 patients have already died from hospital-acquired COVID-19 – the true number is likely much higher as less than half of NHS Trusts responded to this Freedom of Information request192.
- A study in a London teaching hospital found that mortality rate of hospital-acquired COVID-19 was 13% (9% direct cause, 4% contributing factor)193.
- Hospital acquired COVID infections result in increased length of inpatient stays, increased rates of complications and increased post-operative mortality194-197.
- Incidence of other hospital-acquired infections seems to be increased in patients already infected with COVID-19, likely due to virus’ impacts on the immune system198,199.
- Approximately 50% of patients in hospital with COVID in Wales acquired it whilst in hospital for another reason200.
- Data for hospital-acquired COVID in England is no longer collected, but with COVID protections lacking in both countries rates are likely similar.
- 91% of clinically vulnerable people say they have or would delay/cancel medical appointments due to high COVID-19 risks caused by lack of mask mandates, lack of testing and high community levels201.
- Staff COVID infections result in increased absences, worsening staff shortages202, 203, 204.
- A recent study from October 2024 found 33.6% of UK healthcare workers report symptoms consistent with Long COVID205
The truth is that hospitals have a long history of unnecessary delays to implementing infection control. After Semmelweis proved that handwashing reduced mortality in childbirth, this measure remained controversial and for a time the Vienna hospital where he had worked abandoned mandatory handwashing. Similarly, prior to the AIDS pandemic in the early 1980s, gloves were not commonly worn to prevent contact with infectious body fluids. When first introduced the healthcare community were sceptical and offered some resistance, but nowadays they are simply a part of universal precautions that we don’t think twice about206,207.
Can’t I just stay away from people who are obviously ill?
Sadly, no. People can be infected with and transmit COVID before they develop symptoms, or without developing symptoms at all. It is thought that around 30-40% of people are pre- or asymptomatic while infectious, and around 60% of infections are acquired from people without current symptoms208,209.
The majority of people will make attempts to conceal illness to avoid negative social outcomes and complete work-related achievements. One study found that 75% of people admitted to concealing symptoms, putting others at risk of infection210.
Hasn’t the government and public health always worked to protect our health?
The lack of up-to-date COVID data and transparency on long-term effects means that everyone’s health is put at risk. However, this risk is even greater than average in vulnerable and minority groups, who are suffering the brunt of the ongoing pandemic mismanagement.
- Homeless people are at increased risk of reinfection and are more likely to have comorbidities that increase risk of morbidity and mortality211,212.
- People of colour are at increased risk of acute morbidity and mortality213,214,215.
- LGBT people are significantly more likely to report long covid216,217,218.
- People from a low socioeconomic background and those who work manual jobs, are more likely to die or get long covid214,215,219.
- Disabled people and those with pre-existing health conditions are more likely to die from initial infection and more likely to report long covid214,215.
Additionally, a recent Freedom of Information request to the UKHSA has shown that current guidance for children with COVID to isolate for only 3 days is not based on evidence – in fact the paper provided as support for this policy concluded that children are most infectious within the first 5 days220.
If all this is true, aren’t there people trying to raise the alarm?
Yes, communities of people around the world consisting of doctors, scientists, engineers, and non-experts are trying to inform people about the ongoing COVID pandemic.
Organisations and resources that have been created include:
- The World Health Network – a global network of experts and advocates with the aim of ending the pandemic as a global health threat221.
- The John Snow Project – provides reliable, honest information on COVID-19 from public health, clinical, and research experts222.
- The COVID-19 Safety Pledge – Encourages and promotes organisations who have signed the COVID-19 Safety Pledge. This means they pledge to protect workers, service users and customers from COVID-19 through risk assessments to reduce transmission and support for employees to self-isolate. This organisation also runs a Campaign for Safe Healthcare223.
- COVIDhealthimpacts.co.uk – provides peer-reviewed COVID-19 research, summarized briefly in one place. Language aimed to best communicate with all people, regardless of whether they have a scientific background224.
- Clean Air Stars – provide guides for businesses on how to clean the air and promote businesses with cleaner air in their directory225.
- Clean Air Crew – A sourced collection of tips and tools for navigating an airborne pandemic. Focuses on clean air, better masks and school safety226.
- Country-wide mask blocs, including London, Brighton, Norwich, Manchester, Lincoln, Edinburgh and Glasgow – Provide free, high quality masks to those in need227-233.
- COVID Action Map – an interactive map of COVID action groups worldwide, including mask blocs, virtual networks, advocacy organisations, clean air organisations and community events234.
- Protect the Heart of the Arts – grassroots advocacy campaign to sound the alarm on the Long COVID emergency in the performing arts community. They advocate for layered mitigations in venues, like clean air and masking, so that performers, crew, venue staff and patrons can safely attend235.
There many healthcare workers trying to raise the alarm, in the UK these include:
- Dr Claire Taylor – specialist in Long COVID236.
- Dr Rae Duncan – consultant Cardiologist and Long COVID Researcher237
- Prof Nisreen Alwan – public Health Professor MBE238
- Dr Deepti Gurdasani – clinical epidemiologist and statistical geneticist. She recently moved to Australia in the hopes of better COVID safety but still uses social media to speak about conditions in the UK239.
- Prof Tom Lawton – consultant in critical care240.
- Dr David Tomlinson – consultant cardiologist241.
- Prof Trisha Greenhalgh – professor of primary healthcare242.
- Dr Binita Kane – pulmonologist with interest in Long COVID243.
- Dr Helen Salisbury – general practitioner244.
- Dr Jonathan Fluxman – general practitioner245.
UK charities and groups advocating for COVID protections include:
- Clinically Vulnerable Families246
- Long COVID Support247
- Long COVID Kids248
- Long COVID SOS249
- Long COVID Doctors 4 Action250
- Long COVID Nurses and Midwives UK251
- Doctors in Unite252
- COVID-19 Bereaved Families for Justice UK253
- Hazards Campaign254
- COVID Action UK255
However, these voices are overpowered by the mainstream media, who continue to insist that COVID is mild, that the pandemic is over and to mock and belittle those who continue to try to avoid infection.
What can I do to protect myself and others?
Minimise Infections! New infections bear new risks…
- Wear a well-fitted FFP2/3 respirator mask indoors and in outdoor crowds. These are designed to filter airborne viruses, unlike surgical or cloth masks256,257.
- Test regularly, especially before gatherings. Doing so regularly can help reduce your risk of transmitting the virus, but be aware that a negative test does not guarantee that you are free from COVID258.
- Be aware that the full range of COVID symptoms includes muscle pains, sore throat, diarrhoea, vomiting, rashes and conjunctivitis; and that fever, loss of smell and a dry cough are not always present259,260,261.
- Move activities outside if possible and increase indoor ventilation by by opening doors and windows and try to limit time indoors in busy spaces262,263.
- Seek out venues with air filtration – filters such as HEPA filters can be used to physically remove viral particles from the air and significantly reduce risk of infection262,263,264.
- It is possible to use nasal sprays such as Boots Dual Defence/Viraleze and CPC mouthwashes as a complement to masking. While the evidence is limited, so don’t rely on these to prevent infection, they may provide an extra layer of protection265.
- Spread the word – if public health and the government won’t save us, we need to save ourselves.
- Be visible on social media wearing a mask and practising COVID mitigation.
- Share posts and articles on social media which accurately warn of COVID risks.
- Sign and share petitions for universal masking in healthcare and on public transport.
- Amplify the voices of charities/organisations fighting for COVID protections.
If you are infected:
- Isolate for at least 10 days and until you test negative188,266.
- If you must go out anywhere, wear a high quality, well fitted mask188,266.
- Inform those you have recently been in contact with that you have tested positive, and they may have been exposed to COVID188,266.
- Rest as much as possible – this can help to reduce risk of developing Long COVID54.
- Try to isolate from others within the household. Wear a mask, run air filters, and open windows. It is possible to stop household transmission267.
- Try to isolate from pets as much as possible as they can also catch COVID. Studies show that in some cases this can cause multiorgan damage, including brain damage in dogs and cats, and in rare cases death267-271.
- Be vigilant to signs and symptoms of Long COVID, which may develop weeks to months after the initial infection272.
If you have read this far, thank you. I understand that it may seem like the easiest thing to do is bury your head in the sand. Especially if you have already had COVID, it can be scary to think of the damage that might have already been done. But it is possible to prevent transmission and limit any further damage. Avoiding further reinfection can go a long way toward protecting your health, and the health of those you are close with. Our government and public health are not coming to save us – it is up to us to protect our communities. Every infection prevented is health, and potentially a life, saved.
Sources
1. https://whn.global/scientific/sars-cov-2-and-covid-19-from-crisis-to-solution/
2. https://www.who.int/europe/emergencies/situations/covid-19 (accessed 1/2/24)
3. https://www.salon.com/2024/01/04/leader-says-19-is-still-a-pandemic/ (accessed 1/2/2024)
5. https://health-study.zoe.com/data (accessed 1/2/2024)
6. https://scotland.shinyapps.io/phs-respiratory-covid-19/ (accessed 1/2/2024)
7. https://coronadashboard.government.nl/landelijk/rioolwater (accessed 1/2/2024)
8. https://www.cdc.gov/nwss/rv/COVID19-currentlevels.html (accessed 1/2/2024)
9. https://health-infobase.canada.ca/covid-19/wastewater/ (accessed 1/2/2024)
10. https://coronavirus.data.gov.uk/details/healthcare (accessed 1/2/2024)
11. www.gov.uk/coronavirus (accessed 1/2/2024)
12. https://www.gov.uk/government/news/covid-19-testing-approach-from-april-2023 (accessed 1/2/2024)
13. Frediani, Jennifer K, et al. “The New Normal: Delayed Peak SARS-CoV-2 Viral Loads Relative to Symptom Onset and Implications for COVID-19 Testing Programs.” Clinical Infectious Diseases, 28 Sept. 2023, https://doi.org/10.1093/cid/ciad582.
14. https://www.imperial.ac.uk/news/234154/lateral-flow-tests-missing-substantial-number/ (accessed 2/3/24)
15. Dinnes, Jacqueline, et al. “Rapid, Point-of-Care Antigen Tests for Diagnosis of SARS-CoV-2 Infection.” Cochrane Database of Systematic Reviews, vol. 2022, no. 7, 22 July 2022, https://doi.org/10.1002/14651858.cd013705.pub3.
16. https://medriva.com/health/new-covid-variant-triggers-symptoms-before-positive-tests-complicating-diagnoses (accessed 2/3/24)
18. https://www.bbc.co.uk/news/uk-wales-politics-66400511 (accessed 23/5/24)
19. https://data.who.int/dashboards/covid19/wastewater (accessed 23/5/24)
20. https://twitter.com/drclairetaylor/status/1737130371496432074 Dr Claire Taylor Tweet: “Data on reinfections is absolutely vital @UKHSA How is the winter study using lateral flow tests ( check; false negatives up to 50% in first 4 days) going? The population is being hammered by COVID. You are the health security agency.”
21. https://twitter.com/BuDs_UK/status/1745473551434461333 Buckinghamshire Disability Service Tweet: “Why has UKHSA changed their modelling of the Winter Infection Survey (WIS) data to, apparently, make the Christmas & New Year COVID peak ‘vanish’? A short thread:”
22. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (accessed 1/2/2024)
23. https://www.statista.com/statistics/1131428/excess-deaths-in-england-and-wales/ (accessed 1/2/2024)
24. Tan CY, Chiew CJ, Pang D, Lee VJ, Ong B, Lye DC, et al. Protective immunity of SARS-COV-2 infection and vaccines against medically attended symptomatic Omicron Ba.4, BA.5, and XBB Reinfections in Singapore: A national cohort study. The Lancet Infectious Diseases. 2023. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(23)00060-9/fulltext
25. Ren X, Zhou J, Guo J, Hao C, Zheng M, Zhang R, et al. Reinfection in patients with COVID-19: a systematic review. Glob Health Res Policy [Internet]. 2022;7(1):12. Available from: http://dx.doi.org/10.1186/s41256-022-00245-3
26. Girardi V, Gularte JS, Demoliner M, da Silva MS, Filippi M, de Abreu Góes Pereira VM, et al. Reinfection by SARS-CoV-2 by divergent Omicron sublineages, 16 days apart. Braz J Microbiol [Internet]. 2023. Available from: http://dx.doi.org/10.1007/s42770-023-01018-x
27. Ao, D., He, X., Hong, W. and Wei, X. (2023). The rapid rise of SARS‐CoV‐2 Omicron subvariants with immune evasion properties: XBB.1.5 and BQ.1.1 subvariants. MedComm, 4(2). doi: https://doi.org/10.1002/mco2.239.
28. Reuschl, A.-K., Thorne, L.G., Whelan, M.V.X., Ragazzini, R., Furnon, W., Cowton, V.M., De Lorenzo, G., Mesner, D., Turner, J.L.E., Dowgier, G., Bogoda, N., Bonfanti, P., Palmarini, M., Patel, A.H., Jolly, C. and Towers, G.J. (2024). Evolution of enhanced innate immune suppression by SARS-CoV-2 Omicron subvariants. Nature Microbiology, [online] pp.1–13. doi: https://doi.org/10.1038/s41564-023-01588-4.
29. Ferdinands JM, Rao S, Dixon BE, Mitchell PK, DeSilva MB, Irving SA, et al. Waning of vaccine effectiveness against moderate and severe COVID-19 among adults in the US from the Vision Network: Test Negative, case-control study. BMJ. 2022. https://www.bmj.com/content/379/bmj-2022-072141
30. Morens DM, Folkers GK, Fauci AS. The concept of classical herd immunity may not apply to COVID-19. J Infect Dis [Internet]. 2022;226(2):195–8. Available from: http://dx.doi.org/10.1093/infdis/jiac109
31. Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature [Internet]. 2021;591(7851):520–2. Available from: http://dx.doi.org/10.1038/d41586-021-00728-2
32. Janardhan, Vallabh, Janardhan, Vikram and Kalousek, V. (2020) ‘COVID‐19 as a blood clotting disorder masquerading as a respiratory illness: A cerebrovascular perspective and therapeutic implications for stroke thrombectomy’, Journal of Neuroimaging, 30(5), pp. 555–561. doi:10.1111/jon.12770.
33. Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-COV-2 infection. Nature Medicine. 2022;28(7):1461–7.
34. Qasmieh SA, Robertson MKM, Teasdale CA, Kulkarni SG, Jones H, McNairy M, et al. The prevalence of SARS-COV-2 infection and long covid in US adults during the BA.5 Surge, June-July 2022. 2022
35. WHO. Post COVID-19 condition (Long COVID) [Internet]. www.who.int. 2022. Available from: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition
36. Bearne S. Long COVID: what are you entitled to if you can’t work in the UK? The Guardian [Internet]. 2021 Oct 16 [cited 2023 Jun 9]; Available from: http://theguardian.com/society/2021/oct/16/long-covid-what-are-you-entitled-to-if-you-cant-work-in-the-uk
37. Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nature Medicine [Internet]. 2022 Feb 7;28(28):1–8. Available from: https://www.nature.com/articles/s41591-022-01689-3
38. Katsoularis I, Fonseca-Rodríguez O, Farrington P, Jerndal H, Lundevaller EH, Sund M, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ [Internet]. 2022 Apr 6;377:e069590. Available from: https://www.bmj.com/content/377/bmj-2021-069590
39. Tu TM, Seet CYH, Koh JS, Tham CH, Chiew HJ, De Leon JA, et al. Acute Ischemic Stroke During the Convalescent Phase of Asymptomatic COVID-2019 Infection in Men. JAMA Network Open [Internet]. 2021 Apr 22;4(4):e217498–8. Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779040
40. Katsoularis I, Fonseca-Rodríguez O, Farrington P, Lindmark K, Connolly AMF. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. The Lancet [Internet]. 2021 Aug 14;398(10300):599–607. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00896-5/fulltext
41. John Hopkins Medicine. Smoking and Cardiovascular Disease [Internet]. John Hopkins Medicine. 2019. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/smoking-and-cardiovascular-disease
42. Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022 Mar 7;604
43. Crunfli F, Carregari VC, Veras FP, Silva LS, Nogueira MH, Antunes ASLM, et al. Morphological, cellular, and molecular basis of brain infection in COVID-19 patients. Proceedings of the National Academy of Sciences of the United States of America [Internet]. 2022 Aug 30;119(35):e2200960119. Available from: https://pubmed.ncbi.nlm.nih.gov/35951647/
44. Carazo S, Skowronski DM, Laforce R, Talbot D, Falcone EL, Laliberté D, et al. Physical, Psychological, and Cognitive Profile of Post-COVID Conditions in Healthcare Workers, Quebec, Canada. Open Forum Infectious Diseases [Internet]. 2022 Aug 1 [cited 2022 Dec 8];9(8):ofac386. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9379818/
45. Hampshire A, Trender W, Chamberlain SR, Jolly AE, Grant JE, Patrick F, et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine [Internet]. 2021 Jul 22;0(0). Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00324-2/fulltext
46. Tesch F, Ehm F, Vivirito A, Wende D, Batram M, Loser F, et al. Incident autoimmune diseases in association with a SARS-CoV-2 infection: A matched cohort study. 2023 Jan 26
47. Chang R, Yen-Ting Chen T, Wang SI, Hung YM, Chen HY, Wei CCJ. Risk of autoimmune diseases in patients with COVID-19: A retrospective cohort study. eClinicalMedicine. 2023 Feb;56:101783
48. Zarifkar P, Peinkhofer C, Benros ME, Kondziella D. Frequency of Neurological Diseases After COVID-19, Influenza A/B and Bacterial Pneumonia. Frontiers in Neurology. 2022 Jun 23;13.
49. Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. The Lancet Psychiatry [Internet]. 2022 Aug 17;0(0). Available from: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
50. Charnley M, Islam S, Bindra GK, Engwirda J, Ratcliffe J, Zhou J, et al. Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19. Nature Communications. 2022 Jun 13;13(1).
51. Shen W, Logue J, Yang P, Baracco L, Elahi M, E. Albert Reece, et al. SARS-CoV-2 invades cognitive centers of the brain and induces Alzheimer’s-like neuropathology. 2022 Feb 1
52. COVID-19 Associated with Long-Term Cognitive Dysfunction, Acceleration of Alzheimer’s Symptoms | AAIC 2021 [Internet]. AAIC. [cited 2023 Jun 11]. Available from: http://aaic.alz.org/releases_2021/covid-19-cognitive-impact.asp
53. Dubey S, Das S, Ghosh R, Dubey MJ, Chakraborty AP, Roy D, et al. The Effects of SARS-CoV-2 Infection on the Cognitive Functioning of Patients with Pre-Existing Dementia. Ávila J, editor. Journal of Alzheimer’s Disease Reports. 2023 Feb 14;7(1):119–28.
54. Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021 Jul;38(38):101019.
55. Shouman K, Vanichkachorn G, Cheshire WP, Suarez MD, Shelly S, Lamotte GJ, et al. Autonomic dysfunction following COVID-19 infection: an early experience. Clinical Autonomic Research. 2021 Apr 16;31(3):385–94
56. Larsen NW, Stiles LE, Shaik R, Schneider L, Muppidi S, Tsui CT, et al. Characterization of Autonomic Symptom Burden in Long COVID: A Global Survey of 2,314 Adults. 2022 Apr 28
57. Mild COVID-19 Linked to Postural Orthostatic Tachycardia Syndrome [Internet]. Consult QD. 2022. Available from: https://consultqd.clevelandclinic.org/mild-covid-19-linked-to-postural-orthostatic-tachycardia-syndrome/
58. Woo, M.S., Shafiq, M., Fitzek, A., Matthias Dottermusch, Hermann Altmeppen, Mohammadi, B., Mayer, C., Lukas Can Bal, Raich, L., Matschke, J., Krasemann, S., Pfefferle, S., Thomas Theo Brehm, Lütgehetmann, M., Schädler, J., Addo, M.M., Schulze, J., Ondruschka, B., Friese, M.A. and Glatzel, M. (2023). Vagus nerve inflammation contributes to dysautonomia in COVID-19. Acta Neuropathologica, 146(3), pp.387–394. doi:https://doi.org/10.1007/s00401-023-02612-x.
59. Kresch E, Achua J, Saltzman R, Khodamoradi K, Arora H, Ibrahim E, et al. COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. The World Journal of Men’s Health. 2021;39(3):466.
60. Sansone A, Mollaioli D, Ciocca G, Colonnello E, Limoncin E, Balercia G, et al. “Mask up to keep it up”: Preliminary evidence of the association between erectile dysfunction and COVID‐19. Andrology. 2021 Mar 30;9(4):1053–9.
61. Harirugsakul K, Wainipitapong S, Phannajit J, Paitoonpong L, Tantiwongse K. Erectile dysfunction among Thai patients with COVID-19 infection. Translational Andrology and Urology. 2021 Dec;10(0):4376–83.
62. Katz J, Yue S, Xue W, Gao H. Increased odds ratio for erectile dysfunction in COVID-19 patients. Journal of Endocrinological Investigation [Internet]. 2021 Nov 30; Available from: https://pubmed.ncbi.nlm.nih.gov/34846719/
63. Hsieh TC, Edwards NC, Bhattacharyya SK, Nitschelm KD, Burnett AL. The Epidemic of COVID-19-Related Erectile Dysfunction: A Scoping Review and Health Care Perspective. Sexual Medicine Reviews. 2021 Sep
64. Adeyemi DH, Odetayo AF, Hamed MA, Akhigbe RE. Impact of COVID 19 on erectile function. The Aging Male. 2022 Aug 4;25(1):202–16
65. Ma X, Guan C, Chen R, Wang Y, Feng S, Wang R, et al. Pathological and molecular examinations of postmortem testis biopsies reveal SARS-CoV-2 infection in the testis and spermatogenesis damage in COVID-19 patients. Cellular & Molecular Immunology [Internet]. 2020 Dec 14 [cited 2020 Dec 15];1–3. Available from: https://www.nature.com/articles/s41423-020-00604-5
66. Best JC, Kuchakulla M, Khodamoradi K, Lima TFN, Frech FS, Achua J, et al. Evaluation of SARS-CoV-2 in Human Semen and Effect on Total Sperm Number: A Prospective Observational Study. The World Journal of Men’s Health. 2021;39.
67. Ghosh S, Parikh S, Nissa MU, Acharjee A, Singh A, Patwa D, et al. Semen Proteomics of COVID-19 Convalescent Men Reveals Disruption of Key Biological Pathways Relevant to Male Reproductive Function. ACS Omega. 2022 Mar 7;7(10):8601–12.
68. Selvaraj K, Ravichandran S, Krishnan S, Radhakrishnan RK, Manickam N, Kandasamy M. Testicular Atrophy and Hypothalamic Pathology in COVID-19: Possibility of the Incidence of Male Infertility and HPG Axis Abnormalities. Reproductive Sciences. 2021 Jan 7
69. Costa G, Samyra M.S.N. Lacerda, de A, Natalia Teixeira Wnuk, Brener MR, Gabriel Henrique Campolina-Silva, et al. SARS-CoV-2 infects, replicates, elevates angiotensin II and activates immune cells in human testes. 2022 Feb 8
70. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine. 2020 Feb 28;382(18).
71. Shen XR, Geng R, Li Q, Chen Y, Li SF, Wang Q, et al. ACE2-independent infection of T lymphocytes by SARS-CoV-2. Signal Transduction and Targeted Therapy. 2022 Mar 11;7(1).
72. Jing Y, Luo L, Chen Y, Westerberg LS, Zhou P, Xu Z, et al. SARS-CoV-2 infection causes immunodeficiency in recovered patients by downregulating CD19 expression in B cells via enhancing B-cell metabolism. Signal Transduction and Targeted Therapy [Internet]. 2021 Sep 22;6(1):1–13. Available from: https://www.nature.com/articles/s41392-021-00749-3#citeas
73. Govender M, Hopkins FR, Göransson R, Svanberg C, Shankar EM, Hjorth M, et al. T cell perturbations persist for at least 6 months following hospitalization for COVID-19. Frontiers in Immunology [Internet]. 2022;13:931039. Available from: https://pubmed.ncbi.nlm.nih.gov/36003367/
74. Remy KE, Mazer M, Striker DA, Ellebedy AH, Walton AH, Unsinger J, et al. Severe immunosuppression and not a cytokine storm characterizes COVID-19 infections. JCI Insight. 2020 Sep 3;5(17).
75. André S, Picard M, Cezar R, Roux-Dalvai F, Alleaume-Butaux A, Soundaramourty C, et al. T cell apoptosis characterizes severe COVID-19 disease. Cell Death & Differentiation [Internet]. 2022 Jan 22;1–14.
76. Townsend L, Dyer AH, Naughton A, Kiersey R, Holden D, Gardiner M, et al. Longitudinal Analysis of COVID-19 Patients Shows Age-Associated T Cell Changes Independent of Ongoing Ill-Health. Frontiers in Immunology. 2021 May 7;12.
77. Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nature Immunology [Internet]. 2022 Jan 13;23(2):210–6.
78. Winheim E, Rinke L, Lutz K, Reischer A, Leutbecher A, Wolfram L, et al. Impaired function and delayed regeneration of dendritic cells in COVID-19. Suthar M, editor. PLOS Pathogens. 2021 Oct 6;17(10):e1009742.
79. Ryan FJ, Hope CM, Masavuli MG, Lynn MA, Mekonnen ZA, Yeow AEL, et al. Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection. BMC Medicine. 2022 Jan 14;20(1).
80. Ann-Kathrin Reuschl, Thorne L, Whelan MJ, Mesner D, Ragazzini R, Giulia Dowgier, et al. Enhanced innate immune suppression by SARS-CoV-2 Omicron subvariants BA.4 and BA.5. 2022 Jul 12;
81. Lenart M, Górecka M, Bochenek M, Barreto-Duran E, Artur Szczepański, Gałuszka-Bulaga A, et al. SARS-CoV-2 infection impairs NK cell functions via activation of the LLT1-CD161 axis. 2023 May 23;14.
82. Sah R, Zaman K, Mohanty A, Al-Ahdal T, Awad H, Padhi BK, et al. Respiratory syncytial virus with ongoing COVID-19: is it an emerging threat? Annals of Medicine & Surgery. 2023 Jan;85(1):67–70
83. Wang L, Davis PB, Berger NA, Kaelber DC, Volkow ND, Xu R. Disruption in seasonality, patient characteristics and disparities of respiratory syncytial virus infection among young children in the US during and before the COVID-19 pandemic: 2010-2022. 2022 Nov 29
84. Mizrahi B, Sudry T, Flaks-Manov N, Yehezkelli Y, Kalkstein N, Akiva P, et al. Long covid outcomes at one year after mild SARS-CoV-2 infection: nationwide cohort study. BMJ [Internet]. 2023 Jan 11;380:e072529. Available from: https://www.bmj.com/content/380/bmj-2022-072529
85. Nguyen H-NT, Kawahara M, Vuong C-K, Fukushige M, Yamashita T, Ohneda O. SARS-COV-2 m protein facilitates malignant transformation of breast cancer cells. Frontiers in Oncology. 2022 Jun 7;12. doi:10.3389/fonc.2022.923467
86. Habibzadeh P, Dastsooz H, Eshraghi M, Łos MJ, Klionsky DJ, Ghavami S. Autophagy: The potential link between SARS-COV-2 and cancer. Cancers. 2021 Nov 16;13(22):5721. doi:10.3390/cancers13225721
87. Gómez-Carballa A, Martinón-Torres F, Salas A. Is SARS-COV-2 an oncogenic virus? Journal of Infection. 2022 Aug;85(5):573–607. doi:10.1016/j.jinf.2022.08.005
88. Costanzo M, De Giglio MA, Roviello GN. Deciphering the relationship between SARS-COV-2 and cancer. International Journal of Molecular Sciences. 2023 Mar 25;24(9):7803. doi:10.3390/ijms24097803
89. Rahimmanesh I, Shariati L, Dana N, Esmaeili Y, Vaseghi G, Haghjooy Javanmard S. Cancer occurrence as the upcoming complications of COVID-19. Frontiers in Molecular Biosciences. 2022 Jan 28;8. doi:10.3389/fmolb.2021.813175
90. Saini G, Aneja R. Cancer as a prospective Sequela of Long COVID‐19. BioEssays. 2021 Jun 29;43(6):2000331. doi:10.1002/bies.202000331
91. Klein HE. Kashyap Patel, MD, sees link between covid-19 and cancer progression, calls for more biomarker testing [Internet]. MJH Life Sciences; 2023 [cited 2023 Jun 16]. Available from: https://www.ajmc.com/view/kashyap-patel-md-sees-link-between-covid-19-and-cancer-progression-calls-for-more-biomarker-testing
92. Edlow AG, Castro VM, Shook LL, Kaimal AJ, Perlis RH. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-COV-2 during pregnancy. JAMA Network Open. 2022;5(6). doi:10.1001/jamanetworkopen.2022.15787
93. Jin JC, Ananthanarayanan A, Brown JA, Rager SL, Bram Y, Sanidad KZ, et al. SARS COV-2 detected in neonatal stool remote from maternal COVID-19 during pregnancy. Pediatric Research. 2022;93(5):1375–82. doi:10.1038/s41390-022-02266-7
94. Stoecklein S, Koliogiannis V, Prester T, Kolben T, Jegen M, Hübener C, et al. Effects of SARS-COV-2 on prenatal lung growth assessed by fetal MRI. The Lancet Respiratory Medicine. 2022;10(4). doi:10.1016/s2213-2600(22)00060-1
95. Smith ER, Oakley E, Grandner GW, Ferguson K, Farooq F, Afshar Y, et al. Adverse maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infection: an individual participant data meta-analysis. BMJ Glob Health [Internet]. 2023;8(1):e009495. Available from: http://dx.doi.org/10.1136/bmjgh-2022-009495
96. Vousden N, Ramakrishnan R, Bunch K, Morris E, Simpson N, Gale C, et al. Management and implications of severe COVID-19 in pregnancy in the UK: data from the UK Obstetric Surveillance System national cohort. Acta Obstet Gynecol Scand [Internet]. 2022;101(4):461–70. Available from: http://dx.doi.org/10.1111/aogs.14329
97. Metz TD, Clifton RG, Hughes BL, Sandoval GJ, Grobman WA, Saade GR, et al. Association of SARS-CoV-2 infection with serious maternal morbidity and mortality from obstetric complications. JAMA [Internet]. 2022;327(8):748–59. Available from: http://dx.doi.org/10.1001/jama.2022.1190
98. Gurol-Urganci I, Jardine JE, Carroll F, Draycott T, Dunn G, Fremeaux A, et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: national cohort study. Am J Obstet Gynecol [Internet]. 2021;225(5):522.e1-522.e11. Available from: http://dx.doi.org/10.1016/j.ajog.2021.05.016
99. Sacinti KG, Kalafat E, Sukur YE, Koc A. Increased incidence of first-trimester miscarriage during the COVID-19 pandemic. Ultrasound Obstet Gynecol [Internet]. 2021;57(6):1013–4. Available from: http://dx.doi.org/10.1002/uog.23655
100. Ezgi Yangin Ergon, et al. “The Long-Term Neurodevelopmental Outcomes of Toddlers with SARS-CoV-2 Infection in the Neonatal Period: A Prospective Observational Study.” Italian Journal of Pediatrics, vol. 50, no. 1, 27 Feb. 2024, https://doi.org/10.1186/s13052-024-01609-w. Accessed 2 Mar. 2024.
101. Heiss R, Tan L, Schmidt S, Regensburger AP, Ewert F, Mammadova D, et al. Pulmonary Dysfunction after Pediatric COVID-19. Radiology. 2022 Sep 20
102. Sabatino J, Costanza Di Chiara, Angela Di Candia, Sirico D, Donà D, J Fumanelli, et al. Mid- and Long-Term Atrio-Ventricular Functional Changes in Children after Recovery from COVID-19. 2022 Dec 26;12(1):186–6
103. Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. The Lancet Psychiatry [Internet]. 2022 Aug 17;0(0). Available from: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
104. Cao, X. et al. (2022) ‘Accelerated biological aging in COVID-19 patients’, Nature Communications, 13(1). doi:10.1038/s41467-022-29801-8.
105. Stein, S. R., Ramelli, S. C., Grazioli, A., Chung, J.-Y., Singh, M., Yinda, C. K., Winkler, C. W., Sun, J., Dickey, J. M., Ylaya, K., Ko, S. H., Platt, A. P., Burbelo, P. D., Quezado, M., Pittaluga, S., Purcell, M., Munster, V. J., Belinky, F., Ramos-Benitez, M. J., . . . Chertow, D. S. (2022). SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. https://doi.org/10.1038/s41586-022-05542-y
106. Natarajan, A., Zlitni, S., Brooks, E. F., Vance, S. E., Dahlen, A., Hedlin, H., Park, R. M., Han, A., Schmidtke, D. T., Verma, R., Jacobson, K. B., Parsonnet, J., Bonilla, H. F., Singh, U., Pinsky, B. A., Andrews, J. R., Jagannathan, P., & Bhatt, A. S. (2022). Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med. https://doi.org/10.1016/j.medj.2022.04.001
107. Gaebler, C., Wang, Z., Lorenzi, J. C. C., Muecksch, F., Finkin, S., Tokuyama, M., Cho, A., Jankovic, M., Schaefer-Babajew, D., Oliveira, T. Y., Cipolla, M., Viant, C., Barnes, C. O., Bram, Y., Breton, G., Hägglöf, T., Mendoza, P., Hurley, A., Turroja, M., . . . Nussenzweig, M. C. (2021). Evolution of antibody immunity to SARS-CoV-2. Nature, 591(7851), 639–644. https://doi.org/10.1038/s41586-021-03207-w
108. Goh, D. et al. (2022) Persistence of residual SARS-COV-2 viral antigen and RNA in tissues of patients with long covid-19 [Preprint]. doi:10.21203/rs.3.rs-1379777/v1.
109. Armstrong, L., Collin, J., Mostafa, I., Queen, R., Figueiredo, F. C., & Lako, M. (2021). In the eye of the storm: SARS‐CoV‐2 infection and replication at the ocular surface? STEM CELLS Translational Medicine, 10(7), 976–986. https://doi.org/10.1002/sctm.20-0543
110. Costa, G. M. J., Lacerda, S. M. S. N., Figueiredo, A. F. A., Wnuk, N. T., Brener, M. R. G., Andrade, L. M., Campolina-Silva, G. H., Kauffmann-Zeh, A., Pacifico, L. G. G., Versiani, A. F., Antunes, M. M., Souza, F. R., Cassali, G. D., Caldeira-Brant, A. L., Chiarini-Garcia, H., de Souza, F. G., Costa, V. V., da Fonseca, F. G., Nogueira, M. L., . . . Furtado, M. H. (2023). High SARS-CoV-2 tropism and activation of immune cells in the testes of non-vaccinated deceased COVID-19 patients. BMC Biology, 21(1). https://doi.org/10.1186/s12915-022-01497-8
111. Kresch, E., Achua, J., Saltzman, R., Khodamoradi, K., Arora, H., Ibrahim, E., Kryvenko, O. N., Almeida, V. W., Firdaus, F., Hare, J. M., & Ramasamy, R. (2021). COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. The World Journal of Men’s Health, 39(3), 466. https://doi.org/10.5534/wjmh.210055
112. Appelman, B., Charlton, B. T., Goulding, R. P., Kerkhoff, T. J., Breedveld, E. A., Noort, W., Offringa, C., Bloemers, F. W., van Weeghel, M., Schomakers, B. V., Coelho, P., Posthuma, J. J., Aronica, E., Joost Wiersinga, W., van Vugt, M., & Wüst, R. C. I. (2024). Muscle abnormalities worsen after post-exertional malaise in long COVID. Nature Communications, 15(1). https://doi.org/10.1038/s41467-023-44432-3
113. NGAI, J.C. et al. (2010) ‘The long‐term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status’, Respirology, 15(3), pp. 543–550. doi:10.1111/j.1440-1843.2010.01720.x.
114. Petrosillo, N. et al. (2020) ‘COVID-19, SARS and mers: Are they closely related?’, Clinical Microbiology and Infection, 26(6), pp. 729–734. doi:10.1016/j.cmi.2020.03.026.
115. Bowe, B., Xie, Y. and Al-Aly, Z. (2022) ‘Acute and postacute sequelae associated with SARS-COV-2 reinfection’, Nature Medicine, 28(11), pp. 2398–2405. doi:10.1038/s41591-022-02051-3.
116. Epstein J. WHO official says the more times a person gets COVID-19, the more likely they are to be “unlucky” and get long COVID. Business Insider [Internet]. 2022 Jun 27 [cited 2023 Jun 16]; Available from: https://www.businessinsider.com/who-official-individuals-coronavirus-infection-unlucky-long-covid-2022-6
117. Thaweethai T, Jolley SE, Karlson EW, Levitan EB, Levy B, McComsey GA, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA [Internet]. 2023; Available from: http://dx.doi.org/10.1001/jama.2023.8823
118. Thaweethai, T. et al. (2023a) ‘Development of a definition of postacute sequelae of SARS-COV-2 infection’, JAMA, 329(22), p. 1934. doi:10.1001/jama.2023.8823.
119. https://time.com/6553340/covid-19-reinfection-risk/ (accessed 2/3/24)
120. https://abcnews.go.com/Health/common-cold-symptoms-worse-pandemic/story (accessed 3/2/2024)
121. https://www.itv.com/news/2023-02-17/the-cold-thats-not-covid-is-this-winters-sniffle-worse-and-lasting-longer (accessed 3/2/2024)
122. https://uk.news.yahoo.com/warning-over-brutal-cold-spreading-082320290.html (accessed 3/2/2024)
123. https://www.bbc.co.uk/news/newsbeat-58624295 (accessed 3/2/2024)
124. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023/tb-disease-burden/1-1-tb-incidence (accessed 9/4/24)
125. https://www.gov.uk/government/news/tb-cases-rise-in-england (accessed 9/4/24)
126. https://www.nationalgeographic.com/premium/article/shingles-common-young-people-under-50 (accessed 9/4/24)
127. https://www.cbsnews.com/pittsburgh/news/shingles-cases-on-the-rise-in-younger-patients/ (accessed 9/4/24)
128. https://www.abc.net.au/news/2024-03-21/shingles-cases-increasing-nsw-covid-rise/103600746 (accessed 9/4/24)
129. “Long‐Term Risk of Herpes Zoster Following COVID‐19: A Retrospective Cohort Study of 2 442 686 Patients.” J Med Virol, vol. 95, no. 4, 1 Apr. 2023, https://doi.org/10.1002/jmv.28745. Accessed 1 June 2023.
130. Kohlenberg, A., Monnet, D.L. and Plachouras, D. (2022) ‘Increasing number of cases and outbreaks caused by Candida auris in the EU/EEA, 2020 to 2021’, Eurosurveillance, 27(46). Available at: https://doi.org/10.2807/1560-7917.es.2022.27.46.2200846.
131. Egger, N.B. et al. (2022) ‘The rise of Candida auris: from unique traits to co-infection potential’, Microbial Cell, 9(8), pp. 141–144. Available at: https://doi.org/10.15698/mic2022.08.782.
132. He X, Lv F, Zhang Y, Zu J, Li M, Jiao Y, et al. Excess risk for acute myocardial infarction mortality during the COVID‐19 pandemic. Journal of Medical Virology. 2022;95(1). doi:10.1002/jmv.28187
133. https://www.bloomberg.com/news/articles/2024-01-26/spike-in-uk-middle-aged-deaths-could-hit-life-insurers-aviva-legal-general (accessed 3/2/2024)
134. https://www.n-tv.de/wirtschaft/Studie-Rekord-Krankenstand-fuehrte-zur-Rezession-article24690123.html (accessed 3/2/2024)
135. https://www.health.org.uk/news-and-comment/news/health-foundation-responds-to-ons-update-on-economic-inactivity-due-to-long-term-sickness (accessed 2/3/24)
136. https://www.standard.co.uk/business/business-news/number-of-britons-off-work-due-to-longterm-sickness-hits-record-high-figures-b1067158.html (accessed 3/2/2024)
137. https://www.independent.co.uk/news/health/nhs-waiting-list-record-high-b2428410.html (accessed 3/2/2024)
138. https://www.basingstokegazette.co.uk/news/24085340.hampshire-hospitals-declare-critical-incident/?ref=twtrec (accessed /2/2024)
139. https://www.leicestermercury.co.uk/news/leicester-news/traffic-chaos-lri-critical-incident-9055185 (accessed 3/2/2024)
140. https://www.kgh.nhs.uk/news/critical-incident-declared-2619 (accessed 3/2/2024)
141. https://edsource.org/2023/california-districts-still-see-more-chronic-absenteeism-than-before-pandemic/688787 (accessed 3/2/2024)
142. https://www.theguardian.com/education/2023/may/24/uk-parents-what-is-behind-the-rise-in-school-absences (accessed 3/2/2024)
143. https://www.theguardian.com/education/2023/mar/16/one-in-five-pupils-in-england-were-persistently-absent-in-past-school-year (accessed 3/2/2024)
144. https://www.infectioncontroltoday.com/view/covid-19-traffic-accidents-covid-19-personality-disorder-caused-viral-damage-prefrontal-cortex- (accessed 3/2/2024)
145. https://www.billboard.com/pro/tour-cancellations-covid-19-risks-concert-insurance/ (accessed 3/2/2024)
146. https://news.sky.com/story/pink-forced-to-cancel-concerts-due-to-illness-12988169 (accessed 3/2/2024)
147. https://www.rollingstone.com/music/music-news/orville-peck-postpones-bronco-tour-mental-physical-health-1234775876/ (accessed 3/2/2024)
148. https://www.nme.com/news/music/paramore-cancel-remaining-north-american-tour-dates-due-to-illness-3481115 (accessed 3/2/2024)
149. https://www.foxnews.com/entertainment/ryan-adams-cancels-tour-relentless-illness-credits-sobriety-being-anchor (accessed 3/2/2024)
150. https://twitter.com/Adele/status/1762637287442334150?t=AGHdaGWNGHAz15_SU-2JaA&s=19 A tweet from Adele reading “I love you, I’ll miss you like mad and I’m sorry for the inconvenience x” followed by an image of a text note explaining she has been unwell for a prolonged period and so needs to postpone her tour dates. (Accessed 2/3/24)
151. https://www.soa.org/49b504/globalassets/assets/files/resources/experience-studies/2022/group-life-covid-19-mortality-12-2022.pdf (accessed 3/2/2024)
152. https://www1.racgp.org.au/newsgp/clinical/all-excess-deaths-in-singapore-linked-to-recent-co (accessed 3/2/2024)
153. Amer, Fares, et al. “Association between COVID-19 and Outstanding Academic Performance at a Spanish University.” Archives of Public Health, vol. 81, no. 1, 13 Dec. 2023, https://doi.org/10.1186/s13690-023-01225-w. Accessed 2 Mar. 2024.
154. https://twitter.com/MLS_Dave/status/1756026004869452247?t=u0EaqJ0-xuCfG81jnSseRg&s=19 a tweet by @MLS_Dave that reads “We are seeing so many patients who’ve been infected during this wave showing up in our ED weeks/months later with cardiac issues, strokes, blood clotting issues, uncontrolled glucose levels, etc. SARS-CoV-2 can exacerbate pre-existing health issues & turm them into a crisis.” (Accessed 2/3/24)
155. https://twitter.com/imaginemh/status/1756043626982052162?t=3CmUK4cxD9qSVI5tuXgtcg&s=19 a tweet by @imaginemh that reads “As a provider, I am once again asking y’all to mask up because I’ve seen so many people coming to me for new autoimmune disease, worsening psychiatric symptoms, and vascular issues due to likely fallout from COVID. Please protect yourself from becoming severely disabled!” (Accessed 2/3/24)
156. D’Souza, Daniel, et al. “Incidence of Diabetes in Children and Adolescents during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis.” JAMA Network Open, vol. 6, no. 6, 30 June 2023, p. e2321281, jamanetwork.com/journals/jamanetworkopen/fullarticle/2806712, https://doi.org/10.1001/jamanetworkopen.2023.21281.
157. https://www.bbc.co.uk/news/health-66054946 (Accessed 2/3/24)
158. Qeadan, Fares, et al. “The Associations between COVID-19 Diagnosis, Type 1 Diabetes, and the Risk of Diabetic Ketoacidosis: A Nationwide Cohort from the US Using the Cerner Real-World Data.” PLOS ONE, vol. 17, no. 4, 19 Apr. 2022, p. e0266809, https://doi.org/10.1371/journal.pone.0266809.
159. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/selfreportedcoronaviruscovid19infectionsandassociatedsymptomsenglandandscotland/november2023tomarch2024 (Accessed 5/2/25)
160. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/30march2023 (Accessed 2/3/24)
161. https://www.ft.com/content/0640004d-cc15-481e-90ce-572328305798 (accessed 3/2/2024)
162. https://torontolife.com/city/i-was-appalled-to-see-the-prime-minister-making-those-comments-a-u-of-t-epidemiologist-on-the-myth-of-immunity-debt-and-the-real-reason-everyones-getting-sick/ (accessed 3/2/2024)
163. https://healthydebate.ca/2023/01/topic/debunking-myth-immunity-debt/ (accessed 3/2/2024)
164. Lewis, D., 2021. Why indoor spaces are still prime COVID hotspots. Nature, 592(7852), pp.22-25
165. Zhang et al., 2020. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences, 117(26), pp.14857-14863
166. Wang et al., 2021. How effective is a mask in preventing COVID‐19 infection?. MEDICAL DEVICES & SENSORS, 4(1)
167. Greenhalgh et al., 2021. Rapid evidence review to inform safe return to campus in the context of coronavirus disease 2019 (COVID-19). Wellcome Open Research, 6, p.282
168. https://www.abc.net.au/listen/programs/melbourne-mornings/andrew-miller-covid-airborne-transmission/13317660 (accessed 8/2/2024)
169. Greenhalgh, T., Ozbilgin, M. and Contandriopoulos, D. (2021) ‘Orthodoxy, illusio, and playing the scientific game: a Bourdieusian analysis of infection control science in the COVID-19 pandemic’, Wellcome Open Research, 6, p. 126. Available at: https://doi.org/10.12688/wellcomeopenres.16855.3.
170. https://www.telegraph.co.uk/global-health/science-and-disease/every-medical-authority-failed-realise-covid-airborne-late/ (accessed 8/2/2024)
171. https://doctorsinunite.com/2023/01/26/wheres-the-evidence-dr-nabarro/ (accessed 8/2/2024)
172. Smith, L., West, R., Potts, H.W.W., Amlôt, R., Fear, N.T., G James Rubin and Michie, S. (2023). Factors associated with wearing a facemask in shops in England following removal of a legal requirement to do so during the COVID‐19 pandemic. British Journal of Health Psychology. doi:https://doi.org/10.1111/bjhp.12684.
173. https://twitter.com/ukhomeoffice/status/1755531919356477531?t=Vz-P6pu2OOApU5zYn9n_jw&s=19 a tweet from @ukhomeoffice which reads “No protester should be able to evade justice by wearing a face covering. That’s why we’re banning them. Offenders could receive up to a £1,000 fine and a month in prison.” (Accessed 2/3/24)
174. Zenone, M., Snyder, J., Marcon, A. and Caulfield, T. (2022). Analyzing natural herd immunity media discourse in the United Kingdom and the United States. PLOS Global Public Health, 2(1), p.e0000078. doi:https://doi.org/10.1371/journal.pgph.0000078.
175. https://www.theguardian.com/world/2020/mar/13/herd-immunity-will-the-uks-coronavirus-strategy-work (accessed 23/5/24)
176. https://johnsnowproject.org/fact/the-virus-spreads-in-the-air/ (Accessed 2/3/24)
177. https://www.covidhealthimpacts.co.uk/evidence-that-masks-prevent-spread (Accessed 2/3/24)
178. https://www.phc.ox.ac.uk/news/comprehensive-review-confirms-masks-reduce-covid-19-transmission (accessed 23/5/24)
179. Greenhalgh, T., C. Raina MacIntyre, Baker, M.G., Bhattacharjee, S., Chughtai, A.A., Fisman, D., Mohana Kunasekaran, Kvalsvig, A., Lupton, D., Oliver, M., Essa Tawfiq, Ungrin, M. and Vipond, J. (2024). Masks and respirators for prevention of respiratory infections: a state of the science review. Clinical microbiology reviews. doi:https://doi.org/10.1128/cmr.00124-23.
180. Christie, B. (2023) ‘COVID-19: Bring back mandatory mask wearing in health settings, say Scottish workers’, BMJ, 382, p. p1648. Available at: https://doi.org/10.1136/bmj.p1648.
181. Nerode, N. C. Doctors should not infect patients [Internet]. WHN. 2023 [cited 2023 Jun 16]. Available from: https://whn.global/doctors-should-not-infect-patients/
182. Waters, A. (2023) ‘Long covid: the doctors’ lives destroyed by an illness they caught while doing their jobs’, BMJ, 382, p. p1983. Available at: https://doi.org/10.1136/bmj.p1983.
183. https://www.theguardian.com/world/2023/oct/08/charities-call-on-nhs-england-to-bring-back-covid-precautions-for-staff (accessed 8/2/2024)
184. https://inews.co.uk/news/health/cancer-charity-mandatory-covid-face-masks-hospital-staff-2679436 (accessed 8/2/2024)
185. https://twitter.com/cv_cev/status/1737955383795171653 Tweet by Clinically Vulnerable Families organisation official twitter page “We second @theRCN’s call to @UKHSA for appropriate protections (as recommended by the @WHO) against the latest COVID risks. Respirator Masks AND Universal #MasksInHealthcare…amongst other things…including #CleanAir💨”
186. https://www.rcn.org.uk/magazines/News/uk-covid-jn-1-variant-rcn-seeks-assurance-on-new-ppe-advice-211223 (accessed 8/2/2024)
187. https://www.abc.net.au/news/2024-02-11/patients-catching-covid-hospitals-australia-infection-control/103442806 (Accessed 2/3/24)
188. Advice for the public on COVID-19 – World Health Organization [Internet]. Who.int. [cited 2023 Jun 16]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
189. https://iris.who.int/bitstream/handle/10665/337199/WHO-2019-nCov-IPC_Masks-2020.5-eng.pdf (accessed 8/2/2024)
190. https://twitter.com/mvankerkhove/status/1737392201414410577?t=r-ErysRT-49hVIum5S3Z2Q Tweet by Maria Van Kerkhove, technical lead of WHO COVID-19 response “@CIDRAP for covering this Just wanted to highlight that universal masking in health facilities is not a new @WHO rec for #COVID19 (this has been our rec for years). In our notice, we provided a reminder of WHO’s numerous comprehensive recs to prevent infections & save lives.”
191. https://www.cidrap.umn.edu/covid-19/who-designates-jn1-separate-covid-19-variant-interest (accessed 8/2/2024)
192. mirror.co.uk/news/uk-news/we-need-better-over-14000-28046576 (accessed 8/2/2024)
193. Hawkins LPA, Pallett SJC, Mazzella A, Anton-Vazquez V, Rosas L, Jawad SM, et al. Transmission Dynamics and associated mortality of nosocomial COVID-19 throughout 2021: A retrospective study at a large teaching hospital in London. Journal of Hospital Infection. 2023;133:62–9.
194. Stimson J, Pouwels KB, Hope R, Cooper BS, Presanis AM, Robotham JV. Estimation of the impact of hospital-onset SARS-CoV-2 infections on length of stay in English hospitals using causal inference. BMC Infect Dis [Internet]. 2022;22(1):922. Available from: http://dx.doi.org/10.1186/s12879-022-07870-w
195. Ridwan K, DeVarennes B, Tchervenkov C, Shum-Tim D, Cecere R, Lachapelle K. Postoperative nosocomial COVID-19 infection in cardiac surgery: An uncommon event with high mortality rate. CJC Open [Internet]. 2021;3(10):1217–20. Available from: http://dx.doi.org/10.1016/j.cjco.2021.05.017
196. Forlenza EM, Higgins JDD, Burnett RA, Serino J, Della Valle CJ. COVID-19 infection after total joint arthroplasty is associated with increased complications. J Arthroplasty [Internet]. 2022;37(7S):S457–64. Available from: http://dx.doi.org/10.1016/j.arth.2021.10.023
197. Levitt EB, Patch DA, Mabry S, Terrero A, Jaeger B, Haendel MA, et al. Association between COVID-19 and mortality in hip fracture surgery in the national COVID cohort collaborative (N3C): A retrospective cohort study. J Am Acad Orthop Surg Glob Res Rev [Internet]. 2022;6(1). Available from: http://dx.doi.org/10.5435/JAAOSGlobal-D-21-00282
198. Buetti N, Ruckly S, de Montmollin E, Reignier J, Terzi N, Cohen Y, et al. COVID-19 increased the risk of ICU-acquired bloodstream infections: a case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med [Internet]. 2021;47(2):180–7. Available from: http://dx.doi.org/10.1007/s00134-021-06346-w
199. Sands KE, Blanchard EJ, Fraker S, Korwek K, Cuffe M. Health care-associated infections among hospitalized patients with COVID-19, March 2020-March 2022. JAMA Netw Open [Internet]. 2023;6(4):e238059. Available from: http://dx.doi.org/10.1001/jamanetworkopen.2023.8059
200. https://public.tableau.com/app/profile/public.health.wales.health.protection/viz/COVID-19-Hospitaladmissionsdashboard/COVID-19hospitaladmissionsdashboard?publish=yes (accessed 8/2/2024)
201. Clinically Vulnerable Families [@cv_cev]. Available at: https://twitter.com/cv_cev/status/1618194848703737858
202. Temkin et al., 2021. Effect of a national policy of universal masking and uniform criteria for severe acute respiratory coronavirus virus 2 (SARS-CoV-2) exposure on hospital staff infection and quarantine. Infection Control & Hospital Epidemiology, 43(6), pp.757-763
203. Khorasanee et al., 2021. The effects of COVID-19 on sickness of medical staff across departments: A single centre experience. Clinical Medicine, 21(2), pp.e150-e154
204. theguardian.com/society/2022/jan/24/long-covid-nearly-2m-days-lost-in-nhs-staff-absences-in-england (accessed 8/2/2024)
205. Dempsey B, Blake HA, Madan I, et al. Post COVID-19 syndrome among 5248 healthcare workers in England longitudinal findings from NHS CHECK Occupational and Environmental Medicine 2024;81:471-479
206. Kalu, I., Henderson, D., Weber, D., & Haessler, S. (2023). Back to the future: Redefining “universal precautions” to include masking for all patient encounters. Infection Control & Hospital Epidemiology, 1-2. doi:10.1017/ice.2023.2
207. nationalgeographic.co.uk/science-and-technology/2020/03/wash-your-hands-was-once-controversial-medical-advice (Accessed 2/3/24)
208. Shang, W. et al. (2022) ‘Percentage of Asymptomatic Infections among SARS-CoV-2 Omicron Variant-Positive Individuals: A Systematic Review and Meta-Analysis’, Vaccines, 10(7), p. 1049. Available at: https://doi.org/10.3390/vaccines10071049.
209. Michael A. Johansson et al. (2021) ‘SARS-CoV-2 Transmission From People Without COVID-19 Symptoms’, JAMA Network Open, 4(1). Available at: https://doi.org/10.1001/jamanetworkopen.2020.35057
210. Merrell, W.N., Choi, S. and Ackerman, J.M. (2024) ‘When and Why People Conceal Infectious Disease’, Psychological Science [Preprint]. Available at: https://doi.org/10.1177/09567976231221990
211. https://www.cbc.ca/news/canada/toronto/homeless-people-toronto-covid-reinfection-1.7103879 (accessed 19/2/24)
212. Mosnier, E. et al. (2023) ‘Cumulative incidence of SARS-CoV-2 infection within the homeless population: insights from a city-wide longitudinal study’, BMJ Open, 13(2), pp. e065734–e065734. Available at: https://do.org/10.1136/bmjopen-2022-065734.
213. www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed 19/2/24)
214. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature [Internet]. 2020;584(7821):430–6. Available from: http://dx.doi.org/10.1038/s41586-020-2521-4
215. Subramanian A, Nirantharakumar K, Hughes S, Myles P, Williams T, Gokhale KM, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med [Internet]. 2022;28(8):1706–14. Available from: http://dx.doi.org/10.1038/s41591-022-01909-w
216. https://covidaidcharity.org/advice-and-information/lgbtqia-identities-more-vulnerable-to-long-covid (accessed 19/2/24)
217. Kuehn BM. Sexual minorities have greater COVID-19 risk factors. JAMA [Internet]. 2021;325(12):1136. Available from: http://dx.doi.org/10.1001/jama.2021.3356
218. https://www.transresearch.org.au/post/long-covid (accessed 19/2/24)
219. Shabnam S, Razieh C, Dambha-Miller H, Yates T, Gillies C, Chudasama YV, et al. Socioeconomic inequalities of Long COVID: a retrospective population-based cohort study in the United Kingdom. J R Soc Med [Internet]. 2023;1410768231168377. Available from: http://dx.doi.org/10.1177/01410768231168377
220. https://twitter.com/teppichhai/status/1756603284691780020 a Twitter thread by user @teppichhai beginning “I did an FOI request to UKHSA requesting the research underpinning their guidance that children shouldn’t be tested for SARS-CoV-2, and that they only need to isolate for 3 days following a positive test. They responded. Let’s have a look at their response and the guidance:”
221. https://whn.global/ (accessed 22/2/24)
222. https://johnsnowproject.org/ (accessed 22/2/24)
223. https://covidpledge.uk/ (accessed 22/2/24)
224. https://www.covidhealthimpacts.co.uk/ (accessed 22/2/24)
225. https://cleanairstars.com/ (accessed 22/2/24)
226. https://cleanaircrew.org/ (accessed 22/2/24)
227. https://www.gofundme.com/f/lets-get-masks-for-london (accessed 22/2/24)
228. https://www.instagram.com/masksforlondon/ (accessed 22/2/24)
229. https://www.instagram.com/glasgowmaskbloc/ (accessed 29/9/24)
230. https://www.instagram.com/_brightonmaskbloc/ (accessed 29/9/24)
231. https://www.instagram.com/maskbloclincoln/ (accessed 29/9/24)
232. https://www.instagram.com/maskblocmanchester/ (accessed 29/9/24)
233. https://www.instagram.com/edinmaskbloc/ (accessed 29/9/24)
234. https://www.google.com/maps/d/u/0/viewer (Accessed 2/3/24)
235. https://protecttheheartofthearts.org/ (Accessed 2/3/24)
236. https://www.drclairetaylor.com/ (accessed 22/2/24)
237. https://twitter.com/Sunny_Rae1 (accessed 22/2/24)
238. https://twitter.com/Dr2NisreenAlwan (accessed 22/2/24)
239. https://twitter.com/dgurdasani1 (accessed 22/2/24)
240. https://twitter.com/LawtonTri (accessed 22/2/24)
241. https://twitter.com/DRTomlinsonEP (accessed 22/2/24)
242. https://twitter.com/trishgreenhalgh (accessed 22/2/24)
243. https://twitter.com/BinitaKane (accessed 22/2/24)
244. https://twitter.com/HelenRSalisbury (accessed 22/2/24)
245. https://www.westminsterextra.co.uk/article/medic-warns-government-risking-lives (Accessed 2/3/24)
246. https://www.clinicallyvulnerable.org/ (accessed 22/2/24)
247. https://www.longcovid.org/ (accessed 22/2/24)
248. https://www.longcovidkids.org/ (accessed 22/2/24)
249. https://www.longcovidsos.org/ (accessed 22/2/24)
250. https://uk.linkedin.com/company/lcd4a (accessed 22/2/24)
251. https://teamlcnmuk.wixsite.com/lcnmuk (accessed 22/2/24)
252. https://doctorsinunite.com/ (accessed 22/2/24)
253. https://covidfamiliesforjustice.org/ (accessed 22/2/24)
254. https://www.hazardscampaign.org.uk/ (accessed 22/2/24)
255. https://covidaction.uk/ (accessed 22/2/24)
256. https://www.covidhealthimpacts.co.uk/guide-to-the-best-masks (accessed 22/2/24)
257. https://whn.global/guidelines/masks/ (accessed 22/2/24)
258. https://whn.global/guidelines/testing/ (accessed 22/2/24)
259. https://health-study.zoe.com/post/the-20-symptoms-of-covid-19-to-watch-out-for (accessed 22/2/24)
260. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed 22/2/24)
261. https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/coronavirus-unusual-symptoms/faq-20487367 (accessed 22/2/24)
262. https://whn.global/guidelines/ventilation/ (accessed 22/2/24)
263. https://www.covidhealthimpacts.co.uk/ventilation-and-air-filtration (accessed 22/2/24)
264. https://cleanaircrew.org/air-filters-work/ (accessed 22/2/24)
265. https://www.covidhealthimpacts.co.uk/nasal-sprays-and-mouth-washes (accessed 22/2/24)
266. https://whn.global/guidelines/sick-with-covid/ (accessed 22/2/24)
267. https://whn.global/guidelines/taking-care-of-an-ill-person/ (accessed 22/2/24)
268. Chutchai Piewbang, et al. “Natural SARS-CoV-2 Infection in Dogs: Determination of Viral Loads, Distributions, Localizations, and Pathology.” Acta Tropica, vol. 249, 1 Jan. 2024, pp. 107070–107070, https://doi.org/10.1016/j.actatropica.2023.107070. Accessed 22 Feb. 2024.
269. Kim, Dong-Hwi, et al. “Neurologic Effects of SARS-CoV-2 Transmitted among Dogs – Volume 29, Number 11—November 2023 – Emerging Infectious Diseases Journal – CDC.” Wwwnc.cdc.gov, wwwnc.cdc.gov/eid/article/29/11/23-0804_article, https://doi.org/10.3201/eid2911.230804. Accessed 29 Oct. 2023.
270. Decaro, Nicola, et al. “SARS-CoV-2 Infection in Dogs and Cats: Facts and Speculations.” Frontiers in Veterinary Science, vol. 8, 10 Feb. 2021, https://doi.org/10.3389/fvets.2021.619207. Accessed 7 Sept. 2021.
271. Carpenter, Ann, et al. “Determining the Role of Natural SARS-CoV-2 Infection in the Death of Domestic Pets: 10 Cases (2020-2021).” Journal of the American Veterinary Medical Association, vol. 259, no. 9, 1 Nov. 2021, pp. 1032–1039, pubmed.ncbi.nlm.nih.gov/34647475/, https://doi.org/10.2460/javma.259.9.1032. Accessed 9 Nov. 2021.
272. https://www.longcovid.org/awareness/what-is-long-covid (Accessed 2/3/24)