Special Issue: Monkeypox
Published on June 3, 2022
Cases of Monkeypox Continue to Surge Internationally
In the past few days Monkepox cases have increased by nearly 100 per day globally.
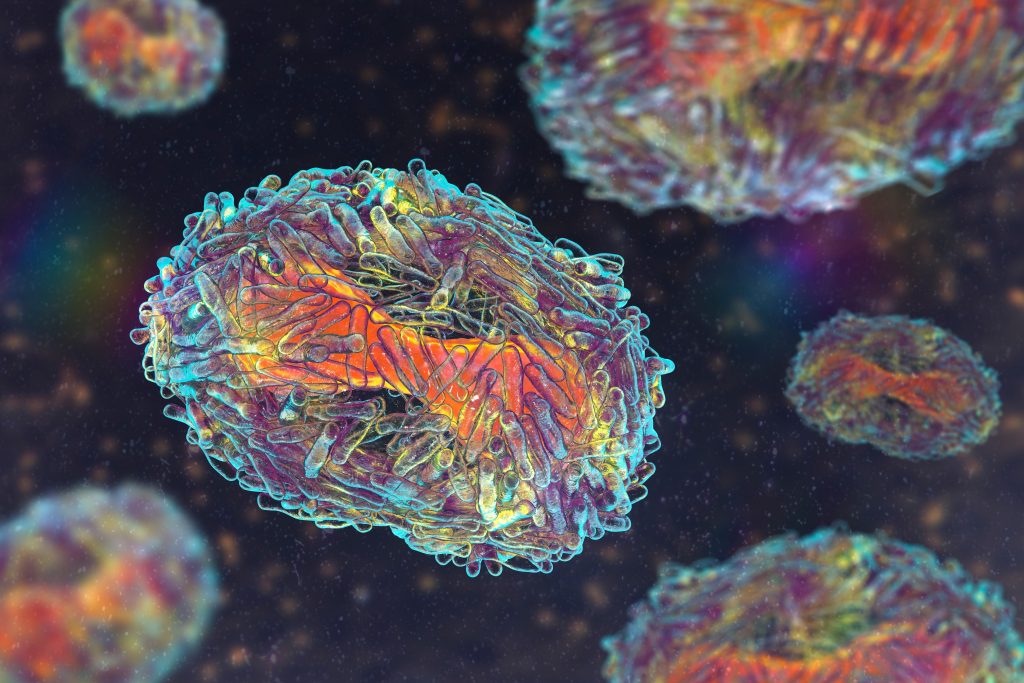
Monkeypox, a virus of the family of orthoviruses, along with smallpox and cowpox, spread internationally after the UK confirmed a case on May 6, 2022. The virus has viral reservoirs in forest mammals in Africa and transmits to humans via bushmeat or contact with infected animals, persons, contaminated air (inhalation of aerosols and droplets), surfaces, and objects. The current spread occurs largely through community transmission. Travel and the relatively long incubation period create conditions for further transmission and more cases will be detected in the coming days and weeks. Smallpox was eradicated by contact tracing and vaccination, and its vaccine is also 85% effective against monkeypox. Discussions are underway about vaccinating portions of the population in multiple countries.
Countries in central Africa have experienced outbreaks of monkeypox over recent decades with increasing numbers of cases reaching over five thousand per year in rural areas where contact with bushmeat occurs. The current outbreak with rapid growth from human to human contact is unprecedented. The outbreak has almost surely been driven by superspreader events in gatherings of the international gay community in Europe. This has led to the expectation that preventing sexual transmission will lead to control of the outbreak. However, it is known that monkeypox transmits through physical contact more generally, contact with contaminated surfaces, and very likely is also airborne. A recent outbreak in Africa included transmission to a taxi driver, ferry operator and nurse, all engaged in infected individual transport. Moreover, travel and social contact in developed countries has a very different network than rural areas of central africa, where village to village contact is more limited, and where there are active efforts to control transmission if the disease is identified. This suggests that we cannot assume the same transmission dynamics will occur, and indeed, observed transmission is already more widespread than gay events alone, with multiple women being infected. In addition to the widely different contact network, reasons for more rapid transmission include mutations (a new variant) and reduced immunity due to widespread COVID infections.
There is no good reason to wait to see if the outbreak is self limiting or continues to spread rapidly. The possibility that the outbreak won’t be self limiting if sexual transmission is avoided provides ample reason to adopt other preventive actions that should include (1) Declaration of the need to report any observation of symptoms consistent with Monkeypox, (2) Intensive contact tracing and vaccination of exposed individuals (which acts as a cure for this disease if done early in its course) and their quarantine.
CHECK IT OUT! Learn about monkeypox and how to protect yourself and your community on our new resource.
Frequently asked questions and circulating misconceptions
- Is monkeypox an STD? No.
Monkeypox can be transmitted via sexual contact, other forms of physical contact, and through other mechanisms including surface and even airborne transmission. - Is the monkeypox outbreak due to sex between men? No.
Transmission of Monkeypox during international meetings of the LGBTQIA+ community resulting in superspreader events, with a large proportion of men being infected, has led to the impression that sex between men is the only significant mode of transmission. However, it is well known that transmission can also occur through other forms of contact, including to women (multiple women have already been infected), and not just through sexual contact. - Does monkeypox affect only people of African descent? No.
Many of the individuals who have been infected during this outbreak are not of African descent. Historical images that have been used in press reports to show the lesions have in some cases led to mistaken claims that only people of African descent can be infected.
RESOURCES
WHAT IS MONKEYPOX?
Monkeypox is an orthopoxvirus, like smallpox and cowpox, which can spread from animals to humans (zoonotic transmission), from human to human, or through contact with contaminated surfaces, objects, or air. Monkeypox is endemic in parts of Africa, with two clades: the Central African Clade, and the Western African Clade. These two strains differ genetically as well as in lethality. The current outbreak is believed to be with the West African strain of the virus.
HOW DO THE TWO KNOWN STRAINS DIFFER?
The Central African strain has a higher lethality rate– approximately 10% of infections result in death, and children are at a higher risk than adults.
The West African strain is associated with ~3% lethality.
Both strains can result in severe disease, defined by the severity of symptoms (rash, fever, neurological complications, respiratory complications). When referring to the West Africa clade as “less severe,” what is meant is that this strain is linked to lower mortality. Symptom severity may still be high.
HOW IS MONKEYPOX TRANSMITTED?
Monkeypox can be transmitted through the following mechanisms:
- Contact with contaminated surfaces and objects
- Inhaling aerosols or droplets containing the virus; aerosols and droplets may also enter through the eyes (in addition to the nose and mouth)
- Person-to-person contact, including:
a. Sharing bodily fluids (sharing food and drinks, sexual contact, kissing, contact with blood)
b. Contact with the rash caused by the virus - Contact with contaminated surfaces
- Consuming contaminated meat or contact with infected animals.
WHAT IS THE COURSE OF THE DISEASE?
The asymptomatic incubation period lasts about 7-14 days. Symptoms initially may include a fever, headache, body aches, chills, and swollen lymph nodes. A rash develops a few days after these initial symptoms, typically on the face and trunk and will spread from there, eventually including the upper body, palms and soles of feet. Lesions are flat at the beginnings, and become elevated and fluid-filled as the disease progresses. In some cases, infected people, especially children, experience neurological and respiratory complications.
WHEN IS A PERSON INFECTIOUS?
The point at which transmission becomes possible is not well established, however, it begins just before or around the time when symptoms begin and lasts until the scabs fall off. Active virus is present in the lesions. Infected individuals remain symptomatic for 2-4 weeks and the infectious period is approximately this long. In some cases, the rash may only occur in one particular area of the body. Therefore, it is important to carefully consider the symptoms to identify suspected cases.
TESTING AND DIAGNOSIS
Diagnosis typically involves examination of clinical symptoms and is confirmed with PCR tests.
PREVENTION
Monkeypox can be transmitted via multiple routes. Experience with smallpox indicates that effective
contact tracing, vaccination of those who are close contacts, and quarantine of those who are infectious is
sufficient to control an outbreak. Belgium has implemented a quarantine policy.
Preventing transmission from a person who may be or is infected requires:
- Avoiding contact during the symptomatic period
- Disinfection of surfaces with 70% ethanol or a solution of 1 tbsp on bleach in 1 gallon of water. Soap and water are insufficient means of disinfection from orthopoxviruses.
- Use of PPE including airborne transmission prevention:
a. high-quality, well-fitting face masks,
b. goggles or other eye protection
c. Ventilation and air purifiers - Avoiding sharing food or drinks
- Vaccines and pharmaceuticals can be used to fight outbreaks, though vaccine immunity is incomplete
Where preventive actions are not being taken to control an outbreak, individual precautions should include:
- Avoiding social gatherings, especially indoors, and physical contact
- Avoiding travel unless necessary
- Isolating if you test positive or suspect exposure. Obtaining a PCR test and informing health authorities and contacts about your diagnosis.
WHY IS THE VIRUS SPREADING SO RAPIDLY?
Travel to and from superspreader events that include gay communities has accelerated the spread of Monkeypox. Additional factors may include virus mutations (conflicting reports here and here) and
reduced immunity due to prior COVID-19 infection. Finally, the social contact network is different in developed countries and potentially much more connected.