COVID Effects on the Brain, a Summary and Resource
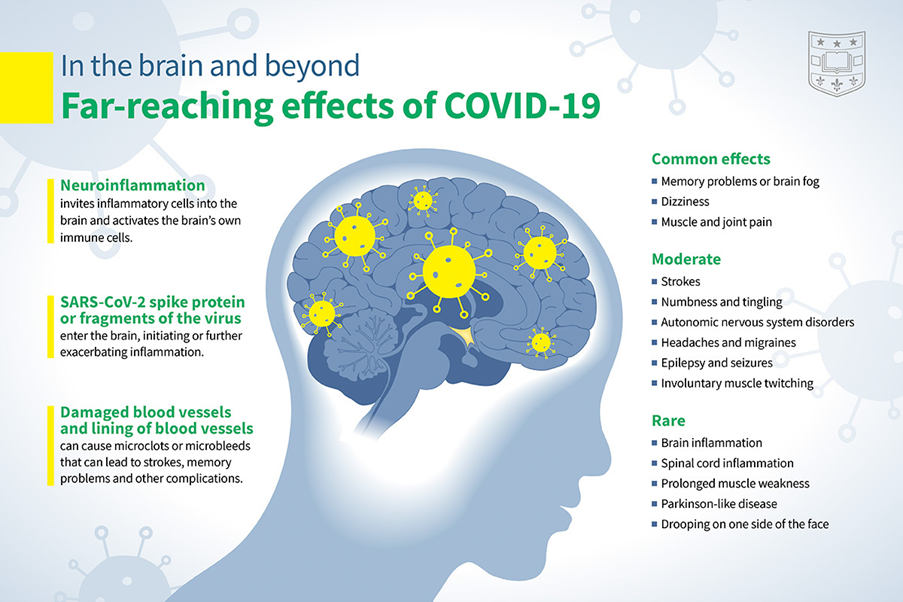
Many studies have now provided strong evidence that the SARS2 virus can enter the brain during infection and cause damage to its function, including loss of both gray and white matter – impacting both the nerve cells and the support cells. In a sense, COVID literally ‘eats’ parts of your brain. It might enter via damaged blood-brain barrier damage as SARS2 damages endothelial cells or it might enter via a nasal nanotube mechanism. Peripheral inflammation has also been shown to lead to post-infection brain deficiency, probably via the release of cytokines. In acute cases the inflammation of brain tissue has been directly observed. All of these occur during the entire spectrum of illness of COVID-19 from mild to severe.
After COVID infection, there are losses in both learning/memory ability and thinking ability, shown in the forms of fluid intelligence. In one study over half of long COVID patients still suffered from forgetfulness and a follow up study showed a dependence on original disease symptoms. In another study, the effects of infection have been shown to affect spatial problem solving, spatial planning, working memory, short-term memory, visual attention, ability to mentally and spatially manipulate objects, reasoning, identify word meaning, and emotion identification. These effects were greatest with higher severity, but some effects were observed for patients even having mild infections. One study showed significant neurologic and psychiatric outcomes of COVID including higher incidence of ischemic stroke, intracranial hemorrhage, plexus disorder, nerve-muscle disease, dementia, and mood/anxiety disorders. Among 236 379 patients diagnosed with COVID-19, the estimated incidence of a neurological or psychiatric diagnosis after 6 months was about 34% with 13% receiving their first such diagnosis. For patients who had serious COVID, the estimated incidence of a diagnosis was 46% and for a first diagnosis was 26%. A huge question is whether COVID infection has not only affected our ability to reason at the individual but also at the population level with social and economic implications.
SARS2 infection can change the brain physically and chemically and evidence indicates that recovery takes years and may not be complete. There is good evidence that at least in severe infections the same chemical structures found in the brains of neurodegerative patients occur (e.g., Parkinson’s disease, Alzheimer’s disease). There is no known way to reverse this degeneration of neurons, and these diseases are considered to be incurable. It is becoming clearer that the number of infections an individual has will be significant in determining the prevalence and perhaps severity of these occurrences. However, we are now finding that even during mild infection, the brain might have lasting changes. Cognitive issues, which include persistent forgetfulness, difficulty with ordering tasks, have been compared to similar changes found in Alzheimer’s disease patients. This connection was suspected early in the pandemic as our sense of smell is located in the same parts of the brain that are changed during Alzheimer’s disease making an association very likely. In a recent study, still in review, Alzheimer’s disease and COVID patients were examined and, adjusting for age and gender, similar molecular and cellular changes were seen. This does not mean COVID infection causes Alzheimer’s disease, but it is fair to state the causal mechanisms might be related in terms of the effect of infection on the brain.
The early assumption that children are safe from COVID was wrong. The effects of COVID on the brain are seen in people of all ages. Several studies have now shown changes in the brains of younger COVID patients. In one study the effects of COVID on children’s brains, ranging from infants to teenagers were examined. In that work, 7 percent of hospitalized kids later developed serious neurological problems, including seizures. These children suffered major brain damage after serious infection, but in another study using positron emission imaging, the brains of children were affected even with mild infections and ensuing long COVID. Brain fog, like that acquired after COVID, is also often associated with concussions and it is well known that multiple concussions compound the problem, so we should not be surprised that multiple infections with SARS Cov2 should be avoided.
The following is a chronological list of some of the research that has been carried out to understand the effects of COVID on the brain. Some potential treatment studies are included.
References on SARS2/COVID Infection and Its Effects on the Brain
(In chronological order)
May 29, 2020, Title: Infectivity of human coronavirus in the brain
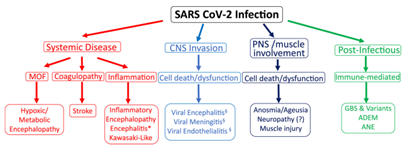
Possible dissemination routes of CNS infection by SARS-CoV-2
https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(20)30174-2/fulltext
July 2020, Title: COVID-19: A Global Threat to the Nervous System
Koralnik and Tyler, ANN NEUROL 2020;88:1–11
https://onlinelibrary.wiley.com/doi/epdf/10.1002/ana.25807
July 17, 2020, Title: Protective Effects of Pituitary Adenylate Cyclase-Activating Polypeptide and Vasoactive Intestinal Peptide Against Cognitive Decline in Neurodegenerative Diseases
Potential treatment based on neurodegenerative disease medications.
“In this review article, we first presented evidence showing the therapeutic potential of PACAP and VIP to fight the cognitive decline observed in models of AD, PD, and HD. We also reviewed the main transduction pathways activated by PACAP and VIP receptors to reduce cognitive dysfunction. Furthermore, we identified the therapeutic targets of PACAP and VIP, and finally, we evaluated different novel synthetic PACAP and VIP analogs as promising pharmacological tools.”
https://doi.org/10.3389/fncel.2020.00221
September 22, 2020, Title: Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19
“Plasma concentrations of blood-based biomarkers for brain damage in patients with mild, moderate, and severe COVID-19 compared to healthy controls”
Neurology 2020;95:e1754-e1759. https://neurology.org/content/neurology/95/12/e1754.full.pdf
November 2020, Title: Anti–SARS-CoV-2 antibodies in the CSF, blood-brain barrier dysfunction, and neurological outcome.
Antibodies in brains of severe covid patients.
January 5, 2021, Title: Alzhheimer’s Foundation call to action
“The chronic neuropsychiatric sequelae of COVID-19: The need for a prospective study of viral impact on brain functioning”
https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.12255
January 21, 2021, Title: COVID Can Cause Forgetfulness, Psychosis, Mania or a Stutter
”The virus induces neurological symptoms that persist long after the pandemic ends”
February 2021, Title: Persistent Brainstem Dysfunction in Long-COVID: A Hypothesis
”The brainstem contains numerous distinct nuclei and subparts that regulate the respiratory, cardiovascular, gastrointestinal, and neurological processes, which can be linked to long-COVID. As neurons do not readily regenerate, brainstem dysfunction may be long-lasting and, thus, is long-COVID. Indeed, brainstem dysfunction has been implicated in other similar disorders, such as chronic pain and migraine and myalgic encephalomyelitis or chronic fatigue syndrome.”
Shin Jie Yong, ACS Chem. Neurosci. 2021, 12, 4, 573–580 https://pubs.acs.org/doi/10.1021/acschemneuro.0c00793
February 2, 2021, Title: Microvascular injury in the brains of patients with Covid-19
“postmortem high-resolution magnetic resonance imaging (magnetic resonance microscopy) of the brains of patients with coronavirus disease 2019 (Covid-19) (median age, 50 years) and histopathological examination that focused on microvascular changes in the olfactory bulb and brain stem.”
Myoung-Hwa Lee, et al, N Engl J Med 2021; 384:481-483
https://www.nejm.org/doi/full/10.1056/NEJMc2033369
April 6, 2021, Title: 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records
‘Several psychiatric outcomes increase after covid infection.’
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(21)00084-5/fulltext
April 12, 2021, Title: Study: A Third of COVID Patients Develop Neuropsychiatric Symptoms
”Patients may have new neuropsychiatric symptoms or worse symptoms of an existing mental illness.”
”The virus may cause brain damage directly through inflammation or through blood clotting.”
https://www.verywellhealth.com/covid-19-psychosis-neurological-symptoms-5176173
May 22, 2021, Title: Global Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19—A Report for the GCS-NeuroCOVID Consortium and the ENERGY Consortium
”These findings suggest that neurological manifestations are prevalent among patients hospitalized with COVID-19 and are associated with higher in-hospital mortality.”
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779759
July 2021, Title: The prevalence of Obstructive Sleep Apnea (OSA) in patients recovering from COVID-19
”detected remarkable high rates of Obstructive Sleep Apnea (OSA) that might explain the common fatigue symptoms”
https://openres.ersjournals.com/content/7/suppl_7/24
July 7, 2021, Title: Documented Effects of Covid-19 Infection on the Brain
“Growing evidence suggests that the coronavirus causes ‘brain fog’ and other neurological symptoms through multiple mechanisms.”
https://www.nature.com/articles/d41586-021-01693-6
July 22, 2021, Title: Cognitive deficits in people who have recovered from Covid-19
“People who had recovered from COVID-19, including those no longer reporting symptoms, exhibited significant cognitive deficits versus controls when controlling for age, gender, education level, income, racial-ethnic group, pre-existing medical disorders, tiredness, depression and anxiety. The deficits were of substantial effect size for people who had been hospitalised (N = 192), but also for non-hospitalised cases who had biological confirmation of COVID-19 infection (N = 326). ”
Adam Hampshire et al., EClinical Medicine 39, 101044, 2021 https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00324-2/fulltext
August 9, 2021, Title: Long covid study. Brain issues
“The five most common symptoms were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), and dyspnea (24%).” & “80% of the infected patients with SARS-CoV-2 developed one or more long-term symptoms.” https://www.nature.com/articles/s41598-021-95565-8
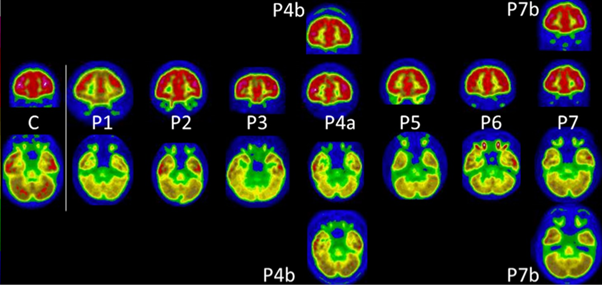
August 19, 2021, Title: Similar patterns of [18F]-FDG brain PET hypometabolism in paediatric and adult patients with long COVID: a paediatric case series
’Similar patterns of 18F-FDG brain PET hypometabolism in children (and adults) with long COVID’
https://link.springer.com/article/10.1007/s00259-021-05528-4
September 2021, Title: Neurocognitive Outcome Following Recovery from Severe Acute Respiratory Syndrome – Coronavirus-1 (SARS-CoV-1)
October 5, 2021, Title: Mechanism of Anosmia Caused by Symptoms of COVID-19 and Emerging Treatments
Potential treatment.
“This paper covers all of the studies investigating olfactory disorders following COVID-19 infection and explains the possible reasons for the correlated anosmia, including olfactory cleft syndrome, local inflammation in the nasal epithelium, early apoptosis of olfactory cells, changes in olfactory cilia and odor transmission, damage to microglial cells, effect on olfactory bulbs, epithelial olfactory injury, and impairment of olfactory neurons and stem cells. The key questions that arise in this field have been discussed, such as why prevalent anosmia is varied among the age categories and among sexes and the correlation of anosmia with mild or severe COVID-19 infection. The angiotensin-converting enzyme 2 receptor is a significant player in the mechanism of anosmia in COVID-19 patients. Based on current studies, a novel approach to treat long-COVID-19 with ongoing anosmia has been proposed. The fields of smart drug delivery, tissue engineering, and cell therapy provide a hypothesized strategy that can minimize the side effects of current treatments and support efficient recovery of the olfactory system.”
Saifalian and coworkers, ACS Chem. Neurosci. 2021, 12, 20, 3795–3805
https://pubs.acs.org/doi/10.1021/acschemneuro.1c00477
October 21, 2021, Title: The SARS-CoV-2 main protease Mpro causes microvascular brain pathology by cleaving NEMO in brain endothelial cells
”Coronavirus disease 2019 (COVID-19) can damage cerebral small vessels and cause neurological symptoms. Here we describe structural changes in cerebral small vessels of patients with COVID-19 and elucidate potential mechanisms underlying the vascular pathology. In brains of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-infected individuals and animal models, we found an increased number of empty basement membrane tubes, so-called string vessels representing remnants of lost capillaries.”
Potential treatment.
Blood vessel and BBB damage. “By ablating NEMO, M pro induces the death of human brain endothelial cells and the occurrence of string vessels in mice. Deletion of receptor-interacting protein kinase (RIPK) 3, a mediator of regulated cell death, blocks the vessel rarefaction and disruption of the blood–brain barrier due to NEMO ablation. Importantly, a pharmacological inhibitor of RIPK signaling prevented the Mpro -induced microvascular pathology. Our data suggest RIPK as a potential therapeutic target to treat the neuropathology of COVID-19.”
Nat Neurosci 24, 1522–1533 (2021). https://doi.org/10.1038/s41593-021-00926-1
November 2021, Title: Counting the neurological cost of COVID-19
Early ideas of how Sars-2 gets into and affects the brain
Nature Reviews Neurology,
https://www.nature.com/articles/s41582-021-00593-7
December 1, 2021, Title: Anti-SARS-CoV-2 and Autoantibody Profiles in the Cerebrospinal Fluid of 3 Teenaged Patients With COVID-19 and Subacute Neuropsychiatric Symptoms Potential treatment.
“Pediatric patients with COVID-19 and prominent subacute neuropsychiatric symptoms, ranging from severe anxiety to delusional psychosis, may have anti–SARS-CoV-2 and antineural antibodies in their CSF and may respond to immunotherapy.”
JAMA Neurol. 2021;78(12):1503-1509
https://jamanetwork.com/journals/jamaneurology/fullarticle/2785032
December 3, 2021, Title: Interactions between SARS-CoV-2 N-Protein and α-Synuclein Accelerate Amyloid Formation
“Our results point toward direct interactions between the N-protein of SARS-CoV-2 and α-synuclein as molecular basis for the observed correlation between SARS-CoV-2 infections and Parkinsonism.”
ACS Chem. Neurosci. 2022, 13, 1, 143-150 https://pubs.acs.org/doi/10.1021/acschemneuro.1c00666
December 21, 2021, Title: SARS-CoV-2 infection of olfactory epithelial cells and neurons drives acute lung injury and lethal COVID-19 in mice
https://www.biorxiv.org/content/10.1101/2021.12.04.471245v1.full.pdf
January 8, 2022, Title: Risks of mental health outcomes in people with covid-19: cohort study
”The findings suggest that people who survive the acute phase of covid-19 are at increased risk of an array of incident mental health disorders.”
https://www.bmj.com/content/bmj/376/bmj-2021-068993.full.pdf
January 14, 2022, Title: β-Amyloid Deposits in Young COVID Patients
Preprint “describes the unexpected but valuable finding that patients who died as a result of COVID-19 exhibit large amounts of focal β-amyloid deposits in their neocortical tissues upon autopsy. The correlation with the findings from the brains of non-COVID-19 patients who experienced markedly hypoxic conditions indicates that the amyloid deposition is not a specific sign of SARS-CoV-2 infection, but rather a response to brain hypoxia.” Quote from, “https://www.news-medical.net/news/20220125/Beta-amyloid-deposits-found-in-young-patients-with-COVID-19.aspx”
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4003213
March 7, 2022, Title: SARS-CoV-2 is associated with changes in brain structure in UK Biobank
”We identified significant longitudinal effects when comparing the two groups, including (1) a greater reduction in grey matter thickness and tissue contrast in the orbitofrontal cortex and parahippocampal gyrus; (2) greater changes in markers of tissue damage in regions that are functionally connected to the primary olfactory cortex; and (3) a greater reduction in global brain size in the SARS-CoV-2 cases. The participants who were infected with SARS-CoV-2 also showed on average a greater cognitive decline between the two time points. Importantly, these imaging and cognitive longitudinal effects were still observed after excluding the 15 patients who had been hospitalised.” And “Whether this deleterious effect can be partially reversed, or whether these effects will persist in the long term, remains to be investigated with additional follow-up.”
https://www.nature.com/articles/s41586-022-04569-5
March 17, 2022, Title: COVCOG 1: Factors Predicting Physical, Neurological and Cognitive Symptoms in Long COVID in a Community Sample. A First Publication From the COVID and Cognition Study
”Specifically, we found that neurological/psychiatric and fatigue/mixed symptoms during the initial illness, and that neurological, gastrointestinal, and cardiopulmonary/fatigue symptoms during the ongoing illness, predicted experience of cognitive symptoms.”
https://www.frontiersin.org/articles/10.3389/fnagi.2022.804922/full
March 17, 2022, Title: COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication from the COVID and Cognition Study
” We found a consistent pattern of memory deficits in those that had experienced the COVID-19 infection, with deficits increasing with the severity of self-reported ongoing symptoms. Fatigue/Mixed symptoms during the initial illness and ongoing neurological symptoms were predictive of cognitive performance.”
https://www.frontiersin.org/articles/10.3389/fnagi.2022.804937/full
March 23, 2022, Title: Visual interpretation of brain hypometabolism related to neurological long COVID: a French multicentric experience
”PET scans in long covid patients with neurological symptoms – all had had hypometabolism”
https://link.springer.com/article/10.1007/s00259-022-05753-5
March 31, 2022, Title: SARS-CoV-2 spike protein induces cognitive deficit and anxiety-like behavior in mouse via non-cell autonomous hippocampal neuronal death
”our data suggest a novel pathogenic mechanism for the COVID-19-associated neurological symptoms that involves glia activation and non-cell autonomous hippocampal neuronal death by the brain-infiltrating S1 protein.”
https://www.nature.com/articles/s41598-022-09410-7
April 1, 2022, Title: Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study
”Neurocognitive long-COVID symptoms can persist ≥1 year after COVID-19 symptom onset and reduce life quality significantly. Several neurocognitive symptoms were associated with ANA titer elevations. This may indicate autoimmunity as a cofactor in etiology of long COVID.”
https://doi.org/10. 1093/cid/ciab611
April 8, 2022, Title: Brain Inflammation and Intracellular α-Synuclein Aggregates in Macaques after SARS-CoV-2 Infection
“The heterogeneity of these manifestations in the brains indicates the virus’ neuropathological potential and should be considered a warning for long-term health risks, following SARS-CoV-2 infection.”
https://pubmed.ncbi.nlm.nih.gov/35458506/
May 9, 2022, Title: Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/ Post-Acute Sequelae of COVID-19 (PASC)
Potential treatment.
Treatment of clots and amyloid micro clots, “Each of the 24 treated cases reported that their main symptoms were resolved and fatigue as the main symptom was relieved, and this was also reflected in a decrease of both the fibrin amyloid microclots and platelet pathology scores.” Potential treatment of brain injury.
https://www.researchsquare.com/article/rs-1205453/v2
May 17, 2022, Title: Amyloidogenesis of SARS-CoV-2 Spike Protein
”the results propose taking S-protein amyloidogenesis into account when studying COVID-19 and long COVID-19 symptoms.” Diabetes, neurodegeneration all possible.
https://pubs.acs.org/doi/10.1021/jacs.2c03925
May 20, 2022, Title: SARS-CoV-2 Infects Peripheral and Central Neurons of Mice Before Viremia, Facilitated by Neuropilin-1
”SARS-CoV-2 rapidly invades and establishes productive infection in previously unassessed sites in the nervous system via direct invasion of neurons before viremia, which may underlie some cognitive and sensory symptoms associated with COVID-19.”
https://www.biorxiv.org/content/10.1101/2022.05.20.492834v1
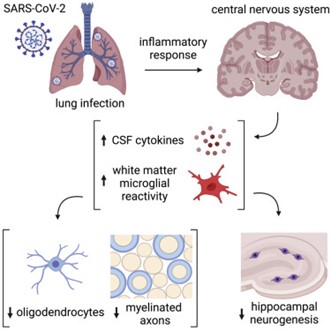
May 25, 2022, Title: Covid and the brain: A neurological health crisis
”Even a mild SARS-CoV-2 infection can cause inflammation that disrupts neural communication, says Stanford neurologist Michelle Monje. Her concern is that Covid-19 may leave millions dealing with cognitive problems, from a loss of mental sharpness to lapses in memory, that prevent them from returning to their previous level of function.”
https://knowablemagazine.org/article/health-disease/2022/covid-and-brain-neurological-health-crisis
May 26, 2022, Title: Mental health outcomes following COVID-19 infection: Evidence from 11 UK longitudinal population studies
”Self-reporting COVID-19 was longitudinally associated with deterioration in mental health and life satisfaction.”
https://www.medrxiv.org/content/10.1101/2022.05.11.22274964v1
May 26, 2022, Title: Unusual Involvement of Basal Ganglia and Dentate Nucleus in Children with Acute Encephalopathy with COVID-19
”two cases of acute encephalopathy with COVID-19”
https://link.springer.com/article/10.1007/s12098-022-04253-6
June 4, 2022, Title: Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET
”Quantitative measures of binding (BPND values) were increased on average by 121% and 76%, respectively. This implicates profound neuroinflammation in the pathophysiology of long COVID.”
https://www.medrxiv.org/content/10.1101/2022.06.02.22275916v1
June 6, 2022, Title: The unique ORF8 protein from SARS-CoV-2 binds to human dendritic cells and induces a hyper-inflammatory cytokine storm
”a neutralizing antibody that has the capacity of blocking the cytokine and chemokine response mediated by ORF8 protein might be an essential and novel additional step in the therapy of severe SARS-CoV-2 cases.”
https://www.biorxiv.org/content/10.1101/2022.06.06.494969v1
June 7, 2022, Title: Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study
”The KP as a unique biomarker offers a potential therapeutic target for COVID-19-related cognitive impairment.”
https://www.medrxiv.org/content/10.1101/2022.06.07.22276020v1.full
June 10, 2022, Title: Comprehensive clinical assessment identifies specific neurocognitive deficits in working-age patients with long-COVID
” Cognitive assessment identified a specific deficit of the same magnitude as intoxication at the UK drink driving limit or the deterioration expected with 10 years ageing, which appears to contribute significantly to the symptomatology of long-COVID.”
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0267392
June 9 2022, Title: Neurodevelopmental Outcomes at 1 Year in Infants of Mothers Who Tested Positive for SARS-CoV-2 During Pregnancy
”those born to the 222 mothers with a positive SARS-CoV-2 polymerase chain reaction test during pregnancy were more likely to receive a neurodevelopmental diagnosis in the first 12 months after delivery, even after accounting for preterm delivery.”
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2793178
June 12, 2022, Title: Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation
“These findings illustrate similar neuropathophysiology after cancer therapy and respiratory SARS-CoV-2 infection which may contribute to cognitive impairment following even mild COVID.”
https://www.cell.com/cell/fulltext/S0092-8674(22)00713-9
June 13, 2022, Title: Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19
”some neurological symptoms of COVID-19 may follow an amyloid etiology .. two peptides from the SARSCoV-2 proteome .. self-assemble into amyloid assemblies. .. these amyloids .. highly toxic to neuronal cells.”
https://www.nature.com/articles/s41467-022-30932-1.epdf
June 13, 2022, Title: Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels
Potential treatment.
”Molecular modeling analyses complemented by experimental studies in cells showed that SARS-CoV-2 entry in endothelial cells is prevented by melatonin binding to an allosteric-binding site on human angiotensin-converting enzyme 2 (ACE2), thus interfering with ACE2 function as an entry receptor for SARS-CoV-2. Our findings open new perspectives for the repurposing of melatonergic drugs and its clinically used analogs in the prevention of brain infection by SARS-CoV-2 and COVID-19-related long-term neurological symptoms.”
https://link.springer.com/article/10.1007/s00018-022-04390-3
June 24, 2022, Title: Increased levels of circulating neurotoxic metabolites in patients with mild Covid19
”The levels of neurotoxic metabolites were significantly associated with key inflammatory cytokines including IL-6 and TNFα. The COVID-19 risk-factor hypertension was associated with the highest levels of neurotoxic metabolites in plasma. These neuroactive metabolites could be part of the pathological mechanisms underlying cognitive impairment during and post-COVID and should be explored as potential biomarkers for long-COVID symptoms.”
https://www.biorxiv.org/content/10.1101/2022.06.22.497189v1
June 29, 2022, Title: Covid associated with neurodegenerative disorders
Danish obs study: Out of 919,731 individuals that were tested for COVID-19 within the study, researchers found that the 43,375 people who tested positive had a 3.5 times increased risk of being diagnosed with Alzheimer’s disease, 2.6 times with Parkinson’s disease, 2.7 times with ischaemic stroke, and 4.8 times with intracerebral hemorrhage (bleeding in the brain)
https://sciencebasedmedicine.org/covid-associated-with-neurodegenerative-disorders/
https://medicalxpress.com/news/2022-06-covid-positive-patients-higher-neurodegenerative.html
https://www.eurekalert.org/news-releases/956611
July 2022 Evidence that SARS cov2 might build nanotubes from nose cells to brain cells allowing it to shuttle through”Coronavirus may enter the brain by building tiny tunnels from the nose”
July 2022, Title: Neurovascular injury with complement activation and inflammation in COVID-19. Severe “patients had multifocal vascular damage as determined by leakage of serum proteins into the brain parenchyma.”
https://academic.oup.com/brain/advance-article/doi/10.1093/brain/awac151/6621999?login=false
July 5, 2022, Title: Possible cause of long COVID ‘brain fog’ revealed – study. “In the course of their research, scientists found that the neurological effects of long-COVID were strikingly similar to Alzheimer’s and Parkinson’s.”
https://www.jpost.com/health-and-wellness/coronavirus/article-711215
July 5, 2022, Title: COVID-19 Neuropathology: evidence for SARS-CoV-2 invasion of Human Brainstem Nuclei. “Evidence for SARS2 invasion of brain stem nuclei”
https://www.biorxiv.org/content/10.1101/2022.06.29.498117v1
July 5, 2022, Title: Small NIH study reveals how immune response triggered by COVID-19 may damage the brain
”Researchers found evidence of an immune attack after COVID-19 infection that may damage the cells lining the inside of blood vessels in the brain.”

July 5, 2022, Title: Neurovascular injury with complement activation and inflammation in COVID-19
”Antibody-mediated cytotoxicity directed against the endothelial cells is the most likely initiating event that leads to vascular leakage, platelet aggregation, neuroinflammation and neuronal injury. Therapeutic modalities directed against immune complexes should be considered.”
https://academic.oup.com/brain/article/145/7/2555/6621999?login=false
July 15, 2022, Title: SARS-CoV-2 causes brain inflammation via impaired neuro-immune interactions
“administering a non-proliferating adenovirus vector expressing SARS-CoV-2 S1 protein into the nasal cavity of mice, we developed a mouse model (S1 mouse) reproducing brain inflammation, fatigue, depressive symptoms, and lung inflammation”
https://www.biorxiv.org/content/10.1101/2022.07.13.499991v1
July 31, 2022, Title: One-two punch from pair of common viruses may trigger Alzheimer’s disease
”The study also speculates potential future Alzheimer’s problems may arise from the COVID-19 pandemic as SARS-CoV-2 infections have been known to reactivate dormant VSV and HSV-1 infections. ”
https://newatlas.com/health-wellbeing/herpes-shingles-vzv-chicken-pox-alzheimers-disease/
https://content.iospress.com/articles/journal-of-alzheimers-disease/jad220287
August 2022, Title: 3 children with new-onset neurocognitive problems after coronavirus disease 2019 (COVID-19), that showed, at the brain [18F]-fluorodeoxyglucose positron emission tomography/computed tomography, hypometabolism in the left orbito-frontal region.
”The voxel-wise analysis confirmed a cluster of hypometabolic voxels in this region with a peak at −18/46/−4mm (179 voxels, T-Score 8.1). These findings may explain neurocognitive symptoms that some children develop after COVID-19 and require further investigations”
August 5, 2022, Title: Notes from the Field: Increase in Pediatric Intracranial Infections During the COVID-19 Pandemic — Eight Pediatric Hospitals, United States, March 2020–March 2022
https://www.cdc.gov/mmwr/volumes/71/wr/mm7131a4.htm?s_cid=mm7131a4_w#contribAff
August 5, 2022, Title: COVID-19 infection in crucial brain regions may lead to accelerated brain aging
”Major findings include that COVID-19 infections may predispose individuals to developing irreversible neurological conditions, may increase the likelihood of strokes and may increase the chance of developing persistent brain lesions that can lead to brain bleeding.”
https://medicalxpress.com/news/2022-08-covid-infection-crucial-brain-regions.html
August 5, 2022, Title: Long COVID, Cognitive Impairment, and the Stalled Decline in Disability Rates
Discussion of how long covid cognition effects.
August 9, 2022, Title: Loss of Smell Linked to Long Term Covid Cognitive Impairment
W Hazeltine ”a study presented at this year’s Alzheimer’s Association International Conference (AAIC) may have uncovered a key to solving this riddle: loss of smell.”
August 15 2022, Title: COVID-19 and olfactory dysfunction: a looming wave of dementia?
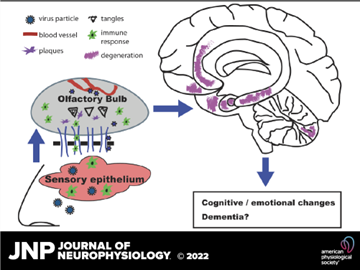
https://journals.physiology.org/doi/full/10.1152/jn.00255.2022
August 31, 2022, Title: Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants, hamster model; “all SARS-CoV-2 variants were found to be neuroinvasive, regardless of the clinical presentation they induce.”
https://www.biorxiv.org/content/10.1101/2022.08.31.505985v1
September 2022, Title: SARS-CoV-2 and the central nervous system: Emerging insights into hemorrhage-associated neurological consequences and therapeutic considerations
”Hemorrhage-mediated neurotoxicity and ageing may synergistically predispose to neurodegeneration/dementia in Covid-19 survivors.”
https://www.sciencedirect.com/science/article/pii/S1568163722001295?via%3Dihub
September 2022, Title: Cognitive-linguistic difficulties in adults with Long COVID
“it is becoming increasingly clear that the true legacy of this crisis in global health may be the very large number of people who do not make a good recovery from COVID-19 infection. The prevalence of so-called Long COVID is beginning to be quantified.”
September 15, 2022, Title: Long COVID Was a Preventable Tragedy. Some of Us Saw It Coming
“between 800,000 and 2.5 million Americans had ME/CFS before the pandemic. Now, with billions of people worldwide having been infected by SARS-CoV-2, the virus that causes COVD-19, the ranks of people whose lives have been upended by post-viral illness has swelled into nearly uncountable millions.”
https://www.webmd.com/lung/news/20220915/long-covid-preventable-tragedy-some-saw-it-coming
September 16, 2022, Title: SARS-CoV-2 and HSV-1 Induce Amyloid Aggregation in Human CSF
”results show that viruses can physically induce amyloid aggregation of proteins in human CSF, and thus providing a potential mechanism that may account for the association between persistent and latent/reactivating brain infections and neurodegenerative diseases”
https://www.biorxiv.org/content/10.1101/2022.09.15.508120v1.full.pdf
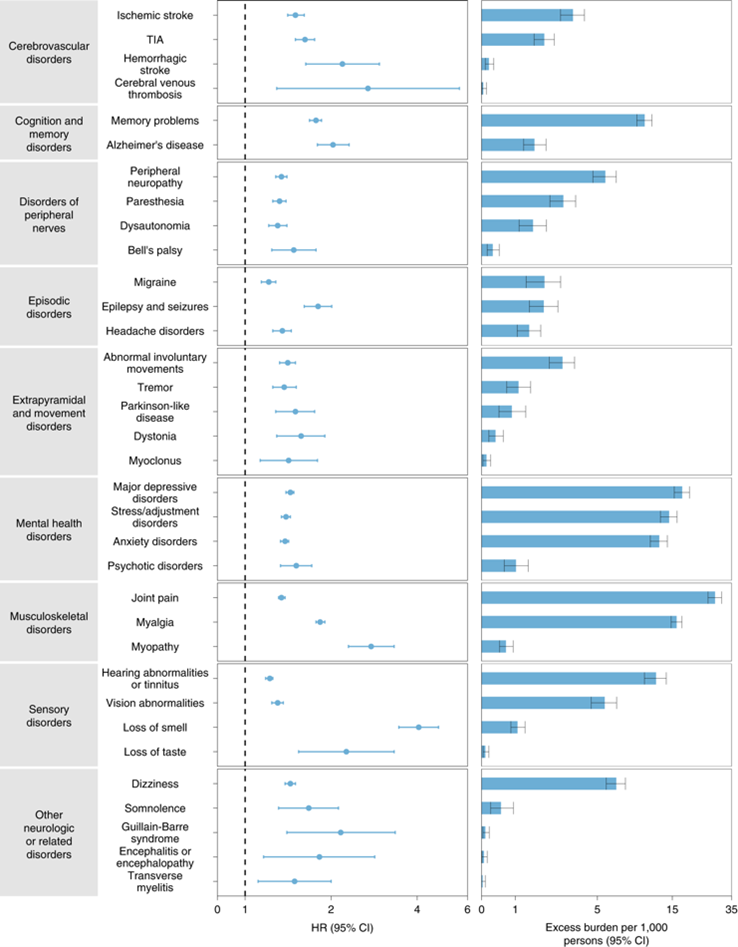
September 22, 2022, Title: Long-term neurologic outcomes of COVID-19
”We estimated that the hazard ratio of any neurologic sequela was 1.42 (95% confidence intervals 1.38, 1.47) and burden 70.69 (95% confidence intervals 63.54, 78.01) per 1,000 persons at 12 months.”
November 12, 2022, Title: Neurologic Conditions Associated with SARS-CoV-2 Infection: A Narrative Review
“We searched three databases for observational and interventional studies in adults published between December 2019 and September 2022. We discussed in narrative form the neurological impairment associated with COVID-19, including clinical signs and symptoms, imaging abnormalities, and the pathophysiology of SARS-CoV2-induced neurological damage.”
https://www.mdpi.com/2076-3425/12/11/1531
https://www.nature.com/articles/s41591-022-02001-z
September 22, 2022, Title: Long-term neurologic outcomes of COVID-19
”Strokes, seizures, memory and movement disorders among problems that develop in first year after infection”
https://doi.org/10.1038/s41591-022-02001-z
September 30, 2022, Title: The impact of a home-based personalized computerized training program on cognitive dysfunction associated with Long COVID: a before-and-after feasibility study
Computer games to help brain fog
https://www.medrxiv.org/content/10.1101/2022.09.28.22280467v1
October 1, 2022, Title: Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients
“risk of psychotic disorder, cognitive deficit, dementia, and epilepsy or seizures persisted throughout”
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
October 5, 2022, Title: Neurogenesis is disrupted in human hippocampal progenitor cells upon exposure to serum samples from hospitalized COVID-19 patients with neurological symptoms
”our results show that serum from COVID-19 patients with delirium can negatively affect hippocampal-dependent neurogenic processes, and that this effect is mediated by IL6-induced production of the downstream inflammatory cytokines IL12 and IL13, which are ultimately responsible for the detrimental cellular outcomes.”
https://www.nature.com/articles/s41380-022-01741-1
October 5, 2022, Title: SARS-CoV-2 promotes microglial synapse elimination in human brain organoids
Normal brains “get rid of a certain amount of inactive synapses…but the infected mini brains showed unnecessarily and inordinate levels of the clean-up process, similar to the level seen in neurological disorders like schizophrenia, Alzheimer’s, and Parkinson’s disease.” During covid, the brain starts destroying internet connections that help brain cells communicate. This explains why a third of people who get Covid end up having problems thinking and concentrating later.”
https://www.nature.com/articles/s41380-022-01786-2.pdf
October 11, 2022, Title: Brain imaging and neuropsychological assessment of individuals recovered from a mild to moderate SARS-CoV-2 infection
White matter is related to MS and is reduced after mild to moderate infection.
https://www.medrxiv.org/content/10.1101/2022.07.08.22277420v3
October 18, 2022, Title: Severe COVID-19 may increase the risk for schizophrenia
”COVID-19 cases that resulted in hospitalization were associated with an 11% increase in risk for developing schizophrenia.”
https://www.psypost.org/2022/10/severe-covid-19-may-increase-the-risk-for-schizophrenia-64088
October 20, 2022, Title: COVID-19 and Acute Neurologic Complications in Children
”Of the 15 137 COVID-19-associated hospitalizations, 1060 (7.0%) children had a neurologic complication. The most common neurologic complication was febrile seizures (582, 3.8%) followed by nonfebrile seizures (352, 2.3%) and encephalopathy (332, 2.1%). The least common neurologic complications were brain abscess or bacterial meningitis (19, 0.13%), and cerebral infarction (8, 0.05%); Reye’s syndrome was not reported.”
October 21, 2022, Title: Long-Haul COVID Patients: Prevalence of POTS Are Reduced but Cerebral Blood Flow Abnormalities Remain Abnormal with Longer Disease Duration
https://www.mdpi.com/2227-9032/10/10/2105/htm
October 21, 2022, Title: T cell responses to SARS-CoV-2 in people with and without neurologic symptoms of long COVID, “Proteomics analysis showed enhanced plasma immunoregulatory proteins and reduced pro-inflammatory and antiviral response proteins in Neuro-PASC patients compared with healthy COVID convalescents, which were also correlated with worse neurocognitive dysfunction. ”
https://www.medrxiv.org/content/10.1101/2021.08.08.21261763v3.full
November 2022, Title: Larger gray matter volumes in neuropsychiatric long-COVID syndrome
In long covid grey matter (nerve cells) increases from inflammation.
https://www.sciencedirect.com/science/article/pii/S0165178122004292?via%3Dihub
November 1, 2022, Title: SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein
”These results support a possible mechanism of microglial innate immune activation by SARS-CoV-2, which could explain the increased vulnerability to developing neurological symptoms akin to Parkinson’s disease in COVID-19 infected individuals, and a potential therapeutic avenue for intervention.”
https://www.nature.com/articles/s41380-022-01831-0
November 2, 2022, Title: Brain 18F-FDG PET imaging in outpatients with post-COVID-19 conditions: findings and associations with clinical characteristics
”A greater number of clinical symptoms during the initial phase of infection and a longer duration of symptoms are risk factors for persistent brain involvement.”
https://link.springer.com/article/10.1007/s00259-022-06013-2#article-info
November 18, 2022, Title: Innate immune response to SARS-CoV-2 infection contributes to neuronal 2 damage in human iPSC-derived peripheral neurons
”Human induced-pluripotent stem cell-derived CNS and PNS neurons with the β strain 40 of were infect with SARS-CoV-2. Our results show that SARS-CoV-2 infects PNS neurons more 41 efficiently than CNS neurons, despite lower expression levels of angiotensin converting 42 enzyme 2. Infected PNS neurons produced interferon λ1, several interferon stimulated 43 genes and proinflammatory cytokines. They also displayed neurodegenerative-like 44 alterations, as indicated by increased levels of sterile alpha and Toll/interleukin 45 receptor motif-containing protein 1, amyloid precursor protein and α-synuclein and 46 lower levels of nicotinamide mononucleotide adenylyltransferase 2 and β-III-tubulin.”
https://www.biorxiv.org/content/10.1101/2022.11.18.517047v1.full.pdf
November 18, 2022, Title: COVID-19 Raises Risk of Seizures, Epilepsy
”Nearly 1 in 100 people infected with COVID-19 developed epilepsy or seizures within 6 months of getting sick”
https://www.webmd.com/lung/news/20221120/covid-19-raises-risk-of-seizures-epilepsy
November 19, 2022, Title: SARS-CoV-2 Infection and Increased Risk for Pediatric Stroke
”The results indicated that stroke is a delayed complication of previous SARS-CoV-2 infections but is not associated with acute infections or MIS-C. Furthermore, stroke is often diagnosed late in pediatric patients due to vague symptoms, delaying treatments and interventions.”
https://www.pedneur.com/article/S0887-8994(22)00210-7/fulltext
November 20, 2022, Title: Enhanced replication of SARS-CoV-2 Omicron BA.2 in human forebrain and midbrain organoids
”The increased efficiency of BA.2 to replicate and causing apoptosis in the brain organoids is alarming, indicating that the long-term consequence of BA.2 infection in the CNS should be closely monitored.” BA.4 and 5 also.
https://www.nature.com/articles/s41392-022-01241-2
November 21, 2022, Title: MRI Reveals Significant Brain Abnormalities Post-COVID
”Researchers identified changes to the brain stem and frontal lobe in patients months after COVID-19 infection.
The affected brain regions are linked with fatigue, insomnia, anxiety, depression, headaches and cognitive problems.”
https://press.rsna.org/timssnet/media/pressreleases/14_pr_target.cfm?id=2381
https://neurosciencenews.com/post-covid-brain-21904/
November 23, 2022, Title: Molecular and cellular similarities in the brain of SARS-CoV-2 and Alzheimer’s disease individuals
”SARS-CoV-2 and Alzheimer’s disease share similar neuroinflammatory processes, which 44 may help explain neuro-PASC”
https://www.biorxiv.org/content/10.1101/2022.11.23.517706v1.full.pdf











