Guidelines for Health Care Settings
SECTION A: Introduction
Health care settings are among the highest risk locations for transmission of infectious disease. Even before the COVID-19 pandemic, infection control in health care settings has been a challenge. The high contact nature of medical care, the large number of and types of roles of individuals who are present and travel from room to room creates an environment of high risk for individual to individual transmission as well as local outbreak conditions. Health care workers are particularly at high risk for being infected, and patients in the hospital for one reason may become infected by another disease.
COVID-19 is a rapidly transmitting disease with approximately 5% of all infections requiring hospitalization during the acute phase and many more requiring care due to post-acute symptoms known as Long COVID. Vulnerable populations include a long list of chronic conditions, as well as pregnancy and absence of vaccination, have higher percentage risk of hospitalization and severe disease.
COVID-19 can transmit with mild symptoms (coughing, sneezing or elevated temperature) and even through asymptomatic persons unaware that they are infected. Reducing the likelihood of transmission is imperative in health care settings.
Here are recommended guidelines for prevention of transmission based on risk mitigation and the precautionary principle. There are five pillars of prevention: Masking, Ventilation and HEPA purification, Testing, Social distancing, and Vaccination. There is also an essential benefit to preventing transmission between parts of facilities, between facilities, or between communities, in reduction of both overall risk and level of precautions that are needed at any one time. Finally, like a fire, the greatest achievement is through local elimination. Wherever this is achieved, the risk level is dramatically reduced and precautions can focus on surveillance. Not allowing a new outbreak becomes a much more targeted effort. We summarize the main suggested strategies to deploy and highlight key items to take into account as of today.
Although this version of the guidelines focuses on applications within traditional hospital and clinic settings, the five-pillar approach can also be applied to other models of care such as pharmacy-based care, dental practices, optometrists, home care, residential care, embedded clinics in industrial workplaces, and other types of facilities such as nursing homes, retirement communities, and prisons.
Principles
- Layered protection: the Swiss Cheese Model of implementing multiple prevention measures to reduce risks and to guard against system failures and errors.
- Sustainability: Protection adequate to prevent transmission over time rather than for individual events.
- Improvement: Elevate protection as the variants become more transmissible due to intrinsic transmissibility and immune evasion.
- Substitution: Options for combining different pillars of prevention by elevating one measure and allowing relaxation of another.
- Upgrading: Individuals may adopt higher levels of protection than is required by the workplace plan, but may not opt for lower levels of protection.
- Training and responsibility: Ensure all workers understand that airborne transmission is the primary mode of transmission of COVID-19 and know what is needed to protect themselves and others
- Clarity: Simplified guides to rules.
Transmission
COVID-19 is primarily transmitted through small airborne particles (aerosols) that float in the air. These particles stay in the air up to several hours, are carried by air currents, and infect others when they are breathed in.
Indirect or secondary routes of transmission include many possibilities for which evidence is more limited, though precautionary measures should be in place, including
- deposits of airborne particles in eyes,
- re-aerosolization from sewage water in bathrooms,
- deposits on food and its consumption,
- deposits on surfaces and subsequent contact to mouth, nose, or face.
We note that the concern about droplet transmission through close proximity and surface transmission has led to inadequate airborne protective measures, instead focusing on surface cleaning, plexiglass barriers without enhanced ventilation/filtration, and 6’ separation. These measures should be reduced in emphasis relative to airborne transmission prevention measures.
Strategy Overview
For safety in healthcare institutions it is important to strengthen daily prevention and control measures as well as strategic organizational and infrastructure guidelines.
Infection control in healthcare settings includes not only protection of workers from patients—under the assumption that patients are the likely source of an infectious disease—but also workers as a likely source of infection, with the potential to spread COVID-19 to patients, visitors, and other workers. Since workers can be infected and infect others, precautions must consider workers as potential vectors of transmission at work, as well as from the healthcare setting to the community, and the community to the healthcare setting, including to and from their own households.
The strategy is designed for implementation of multiple layers (each with different levels of protection and risk reduction). These layers can be combined to achieve effective risk mitigation through the combined effects of multiple measures, which are multiplicative in providing fold-reduction in risk rather than just additive protection. This approach recognizes that all people are at risk of COVID-19 impacts, including Long COVID in addition to acute illness, and that all people should be protected from infection in the workplace.

A comprehensive COVID-19 plan encompasses all activities that workers need access to during the working day and safe transition from and to home, including safe areas for breaks for drinking and meals, bathroom use, and donning and doffing PPE when damaged or soiled. Because PPE must be removed during some activities over the course of the day, increases in other measures will be needed in some spaces to reduce the risk of exposure.
The strategy for infection prevention is based on four pillars: PPE, Testing, Social Distancing, and Air Quality (Ventilation/Filtration). A fifth pillar, Vaccination, is important to reduce severity of disease and death. Additional control methods that support these pillars will also be described. The control methods fall into the well accepted hierarchy of controls consisting of PPE, administrative controls, and engineering controls (See Appendix A).
SECTION B: Five Pillars
The guidelines for prevention of infection are built on five pillars, corresponding to key prevention measures, which are robust and proven risk mitigation measures in various settings. Additional complementary measures to these five can be introduced in specific contexts, but these five pillars are important in essentially all contexts. The existence of multiple components of a transmission prevention strategy enables adapting to local contexts by selecting the level of each of these measures that is adopted.
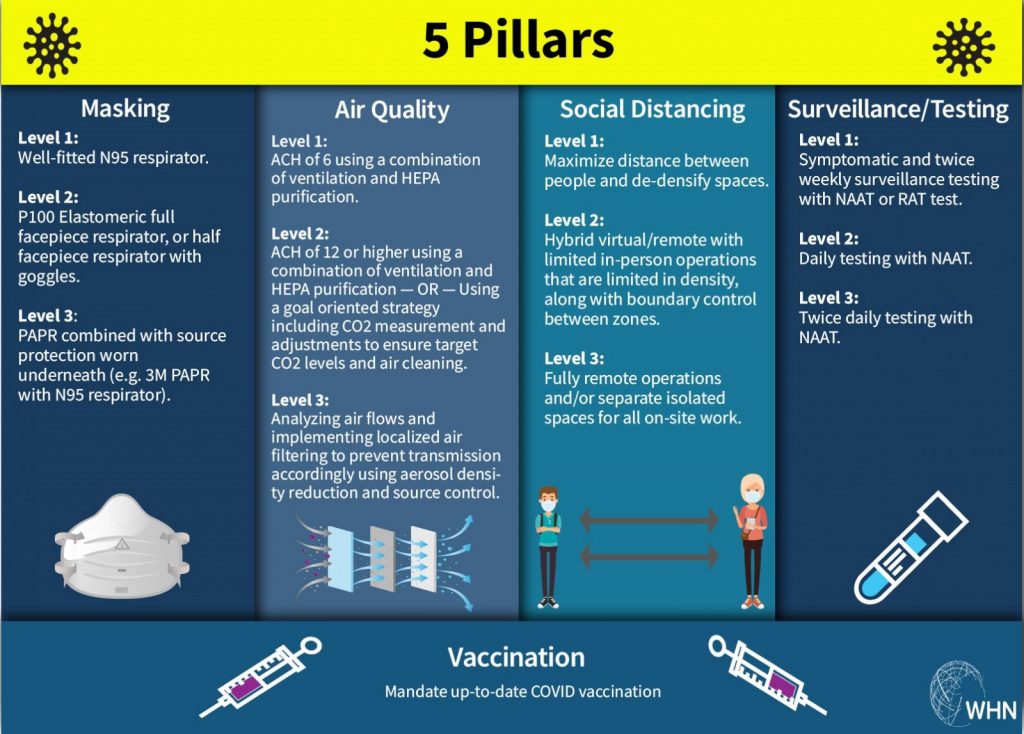
The Five Pillars (methods of preventing transmission)
- Masking
- Air quality (ventilation and air cleaning)
- Testing
- Social distancing
- Vaccination
Of these five pillars, four of the pillars can be implemented at baseline or higher levels to provide increased protection as shown in Table 1.
Note: Pillars can be independently implemented, but once targets of performance are set they become linked. This is true if we establish an overall target of risk reduction requiring combinations of multiple pillars to achieve, or require a particular air quality requiring a combination of occupancy (social distancing) and ventilation or air purification.
| Masking | Air quality (ventilation and air cleaning) | ||
|---|---|---|---|
| Level 1 | Well-fitted N95 respirator | Level 1 | ACH of 6 using a combination of ventilation and HEPA purification |
| Level 2 | P100 Elastomeric full facepiece respirator, or half facepiece respirator with goggles | Level 2 | ACH of 12 or higher using a combination of ventilation and HEPA purification — OR — Using a goal oriented strategy including CO2 measurement and adjustments to ensure target CO2 levels and air cleaning |
| Level 3 | PAPR combined with source protection worn underneath (e.g. 3M PAPR with N95 respirator) | Level 3 | Analyzing air flows and implementing localized air filtering to prevent transmission accordingly using aerosol density reduction and source control |
| Surveillance/Testing | Social distancing | ||
| Level 1 | Symptomatic and twice weekly surveillance testing with NAAT or RAT test | Level 1 | Maximize distance between people and de-densify spaces |
| Level 2 | Daily testing with NAAT | Level 2 | Hybrid virtual/remote with limited in person operations that are limited in density, along with boundary control between zones |
| Level 3 | Twice daily testing with NAAT | Level 3 | Fully remote operations and/or separate isolated spaces for all on-site work |
| Vaccination | |||
| Up-to-date COVID-19 vaccination |
Pillar I: Masking (PPE respiratory protection)
Workers in healthcare settings (Health Care Personnel) must use proper PPE when exposed to any individual whose infection status is unknown (including visitors, patients, and other workers), when exposed to a patient with suspected or confirmed COVID-19, and when exposed to other sources of SARS-CoV-2, where such exposure includes the fact that SARS-COV-2 is airborne and can linger in the air for several hours.
All individuals must wear high quality masks in order to achieve the levels of protection that such masks can provide (risk reduction combines multiplicatively). Individuals wearing high quality masks where others are not wearing masks (i.e. one-way masking), or are wearing low quality masks, are not as well protected. One-way respiratory protection should be avoided as much as possible; when it cannot be avoided, additional risk reduction from higher levels of masking or from other pillars (e.g. enhanced ventilation and filtration) should be implemented to effectively protect workers and patients.
The minimum recommended level of protection is a high quality, well fitted mask — specifically a NIOSH-approved N95 filtering facepiece respirator (see also guidelines on Masks). Higher levels of protection are often warranted especially if optimal engineering controls are not feasible. Traditional surgical masks currently used by the majority of healthcare workers fail to provide effective protection or source control.
In situations where the use of a respirator is not required either by the employer or by an Occupational Safety and Health Administration (OSHA) standard, the employer may still offer filtering facepiece respirators or permit workers to use their own NIOSH-approved respirators as long as the employer determines that such respirator use will not in itself create a hazard.. This is considered voluntary use under the Respiratory Protection Standard. (See OSHA’s PPE standards at |29 CFR 1910 Subpart I).
Notably, the CDC encourages employers to permit workers to voluntarily use filtering facepiece respirators like N95s. If an employer allows voluntary use of filtering facepiece respirators, the employer must provide users with |29 CFR 1910.134 Appendix D – Information for Employees Using Respirators When Not Required Under the Standard. See |29 CFR 1910.134(c)(2) for additional requirements applicable to voluntary respirator use.
But these voluntary based measures should be elevated to strong recommendations or requirements for more specific acute situations. Respiratory protection is primary and should consist of one of three levels of protection depending on level of risk, and complementary measures that are taken.
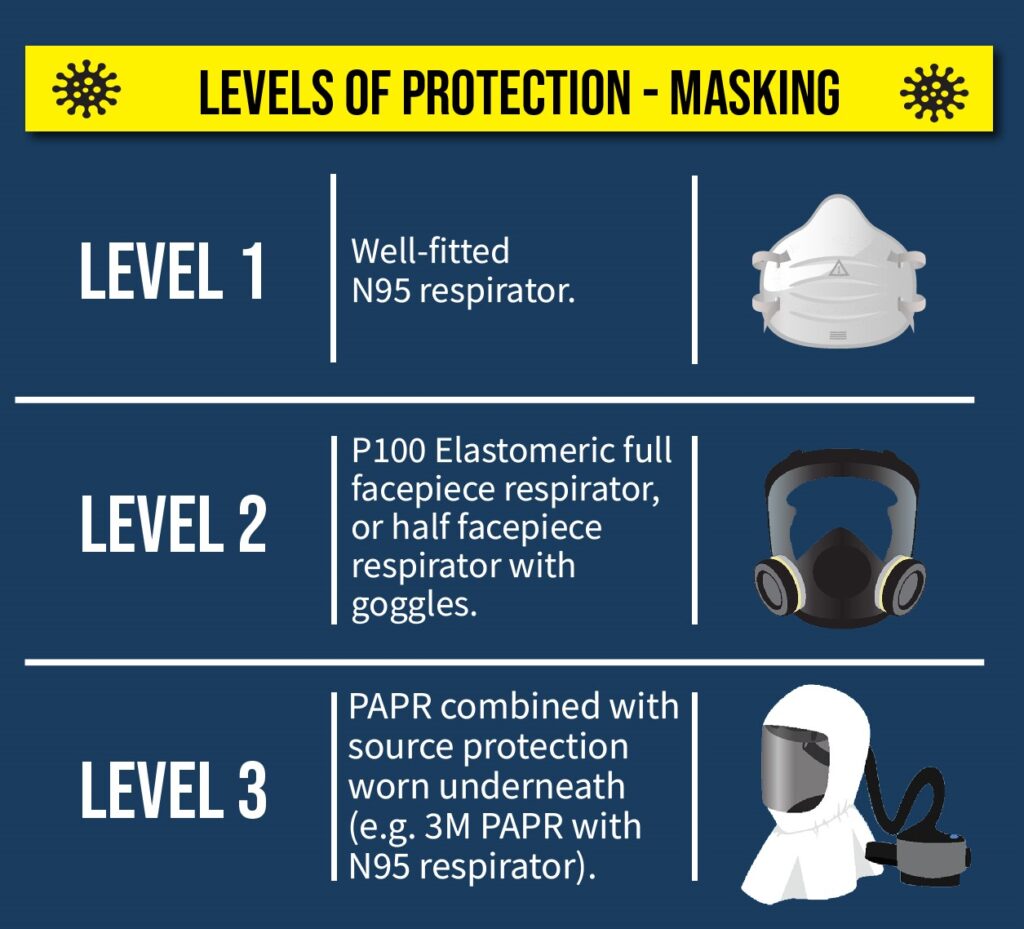
The levels provide varying degrees of protection from COVID-19 transmission. In the context of these guidelines a reference level (Level 0) is no mask, which is only considered acceptable when necessary, as when eating, and other pillars are being used to reduce risk. Level 1 otherwise represents the minimum acceptable level of risk reduction. Increasing levels provide increased levels of protection and risk reduction for both the workers and the patients.
Level 1: Well fitted NIOSH-approved N95 respirators.
Level 2: P100 Elastomeric full facepiece respirator, or half facepiece respirator with source control (e.g. no exhalation valve, blocked exhalation valve, or N95 filter over the exhalation valve), with goggles.
Level 3: NIOSH-approved powered air purifying respirator (PAPR) combined with source protection worn underneath (e.g. N95 respirator)
For example, under conditions where standard measures for ventilation and screening are present, Level (1) N95 respirators should be standard for all encounters with other individuals whose infection status is unknown and in spaces that may have previously been occupied by other individuals over a few hours. Level (2) elastomeric respirators should be standard when exposed to a patient with suspected or confirmed COVID-19. Level (3) PAPRs should be worn for extended time exposure in procedures requiring proximity and aerosol generating procedures. Aerosol generating activities in a healthcare setting include procedures such as intubation, non-invasive positive-pressure ventilation, tracheotomy, bronchoscopy, sputum induction, cardiopulmonary resuscitation, and dental drilling, among others. Aerosol generating procedures create risks under conditions where otherwise airborne precautions are not needed. However, for airborne diseases, infected individuals, symptomatic and asymptomatic, generate aerosols by breathing. Proximity to any individual who’s infection status is known to be infected, or is unknown, should be considered to have risk conditions consistent with an aerosol generating procedure. Hence extended proximity should require the same level of preventive measures. It is also important to remember that the aerosols will remain in the air for several hours after an infected person has left the room.

Levels (2) elastomeric respirator and (3) PAPRs may be considered as a part of any plan but especially should be used under conditions where one of: (a) the workers is clinically vulnerable or wishes to take higher levels of protection, (b) substandard ventilation or (c) substandard screening is present to provide additional protection. PAPRs are highly protective and can be used under elevated risk conditions. Under conditions where two or more of the elements (a,b,c) are present, always use PAPRs. In addition, where individual circumstances limit the effectiveness of masks, e.g. beards or other reasons for fit test failures, either special versions, multiple layers, or higher levels may be needed to achieve adequate levels of protection for them and others. This may also depend on the protections being worn by others in a particular circumstance.
Healthcare personnel, both paid and unpaid, should be allowed to bring their own highly protective masks (such as N95 respirators) as long as the mask does not violate the facility’s safety and health requirements. They should not be asked to remove their more protective source control device (a well-fitting N95 respirator, for example) for a less protective device (such as a procedure mask) unless the mask or respirator is visibly soiled, damaged, or hard to breathe through. However, devices brought from home may not be appropriate for protecting healthcare personnel from all job hazards, and they should change to recommended personal protective equipment when indicated.
In addition to respiratory protection, healthcare workers exposed to suspected or confirmed COVID-19 patients wear:
- Eye/face protection (e.g., goggles, face shields are inadequate)
- Disposable Gowns
- Gloves
Since many individuals have infection status that is unknown, gowns and gloves may be recommended more generally.
A comprehensive respiratory protection program also includes medical exams, fit testing, and training. (|29 CFR 1910.134)
When removing potentially contaminated PPE such as an N95 respirator, do not touch the outside of the respirator without wearing gloves.
PPE for patients and visitors
Patients and visitors should be required to wear PPE due to (1) source control in preventing infection of workers and other patients and visitors, (2) protection from infection by workers and other patients and visitors.
Patients and visitors should wear high quality N95 respirator masks, elastomeric respirators, and PAPRs with source control according to the conditions they are in. Surgical, procedure, or barrier masks do not offer adequate protection or source control for patients and visitors in healthcare settings. Since patients and visitors may not have fit tested masks, they may wear masks that are not fit tested. When possible without risk to workers, patients and visitors should be instructed in proper wearing of masks and fit improving measures such as user checks of fit. Under no circumstances should patients and visitors be required to reduce the level of their mask protection to lower standards, or to cause self exposure through changing PPE, due to institutional standards (e.g., a patient or visitor should not be required to remove an N95 that appears clean and in good repair to don hospital-issued PPE). Institutional standards should be understood as a minimum rather than a maximum requirement.
When a COVID-19 infected patient is resident in a healthcare institution, e.g. for treatment, elevated ventilation and air filtering, and workers masking, should be used instead of patient masking where possible, as rebreathing of viral particles may be detrimental.
Pillar II: Air Quality (Ventilation, HEPA filters, and Monitoring)

This section covers a list of ventilation and other indoor air quality interventions that can help reduce the concentration of virus particles in the air. These tools can be combined in various ways to improve air quality. Implementing multiple tools at the same time increases overall effectiveness and robustness of the mitigation strategies. These engineering control air quality (ventilation plus) interventions can reduce the risk of exposure to the virus and reduce the spread of disease, but they will not eliminate risk completely. The measures in the other sections are necessary to minimize or virtually eliminate the risk.
Healthcare institutions must implement (a) best possible quality building ventilation,(b) identify occupancy limits,(c) the use of CO2 monitors to evaluate ventilation(d) augment with HEPA purification where ventilation is inadequate or risks are high(e) use barriers and ventilation air flows to partition facilities at well-defined boundaries.
Ventilation is needed in order to maintain breathable air by preventing elevated concentrations of CO2. Under most circumstances, CO2 is an indicator of exhaled air, which in turn is an indicator of aerosol infection risk (see Figure 1). Ventilation and air filtering both contribute to reducing risk from airborne particles. Without adequate ventilation, filtered air can be safe from infectious aerosols even though it has a higher level of CO2. However, elevated CO2 levels are also harmful even if the infection risk is low (see Box 1). Thus, CO2 levels should be regulated for both reasons.
| Box 1: Impacts of Indoor Air Quality (including ensuring clean air, proper ventilation, air purification, etc.) on health goes beyond COVID-19. The impact of ventilation on health and especially on cognitive function has been documented. A recent study (Cedeno Laurent et al., 2021, doi: 10.1088/1748-9326/ac1bd8) conducted on 302 office workers in six countries (China, India, Mexico, Thailand, the UK and the US) quantified measurable cognitive effects, including slower response times and reduced accuracy, of the effects of indoor air quality, including particulate pollution and CO2 density on cognitive performance. Improving air quality helps improve the overall health of workers, patients, and visitors. In addition, it positions the facility to better handle potential future infectious disease outbreaks, smoke from wildfires, and air pollution. |

The minimum level of ventilation recommended is 6 Air Exchanges per Hour (ACH). Higher levels of air filtering and quality are often warranted.
Levels of action are given by
Level 1: 6 Air Exchanges per Hour (ACH)
Level 2a: increasing the ACH to 12 or higher using a combination of ventilation and HEPA purification
Level 2b: using a goal oriented strategy: measuring CO2 levels in the space and adjusting fresh air circulation, ventilation, HEPA filtration and occupancy to ensure target CO2 levels. (See additional detail in section below. Note that HEPA filtration alone will not lower CO2 levels as HEPA filters remove airborne particles not gasses from the air.)
Level 3: analyzing air flows and implementing localized air filtering to prevent transmission accordingly, including general reduction of aerosol density as well as suction of exhaled air for source control and directed blowing of filtered air for inhalation protection:(i) placing HEPA filters in area locations where air flows indicates higher benefits of filtering(ii) placing HEPA filters near stationary individuals including HC receptionists, patients in beds, and waiting areas, or locations where patients or visitors are likely to wait, etc.(iii) using HEPA or ULPA air suction equipment such as surgical smoke extractors, dental extraoral suction systems, or negative pressure patient tents.(iv) using HEPA filters placed so their directed outlet air flows to workers, patients or visitors from HEPA filters this can be done using stationary outlet powered HEPA purifiers, or portable battery powered personal HEPA purifiers which can be mounted or hand held and directed toward the holder’s face.(v) placing HEPA filters at boundaries between designated zones of a care facility, including between higher and lower risk areas, or between sections of high risk areas, such as between COVID and non-COVID wards, between patient and non-patient areas, between high traffic and low traffic areas, between dining areas and other spaces, between restrooms and other spaces, between treatment and office areas, between areas of care of nursing stations, and at the boundaries of nursing stations.
Higher levels of ventilation are required where individuals (workers, patients or visitors) are in shared spaces and are unable to use respirators, it is inadvisable to use respirators, or viral laden aerosols are generated, This includes while eating or drinking, dental procedures, surgical procedures, certain medical procedures (see above), as well as COVID-19 infected patients in hospital beds (extended use of respirators by infected individuals is not recommended where unnecessary as rebreathing of viral particles may increase viral load).
We provide additional details on Level 2b in the following section.
Level 2b: Goal oriented ventilation and air filtration
Measuring Carbon Dioxide (CO2) is the best way to judge the amount of exhaled air in an indoor space; higher levels of CO2 indicate a higher percentage of the air in a room has already been breathed by someone else. Indoor CO2 levels should not exceed 800 PPM (if no filtering is used) or 1000 ppm, if significant HVAC or portable HEPA filtering is in use. If an indoor space exceeds the target CO2 limit, a) regularly or continuously monitor, display CO2 levels, and perform one or more of the following actions to bring the space into compliance: b) regulate the maximum occupancy level of the space; c) improve natural or mechanical ventilation of the space; OR d) install portable HEPA air cleaners. More specifically:
(a) Monitor and display CO2 levels —
(i) Publicly viewable CO2 monitoring devices should be installed in all shared indoor spaces (“indoor spaces”).
(ii) Display the safe target CO2 level requirements
(b) Occupancy: Enforce occupancy limits — All indoor spaces must specify occupancy limits based on the ability to ventilate the space to target CO2 levels.
(c) Ventilation:
(i) Require high efficiency air filters — Require the use of MERV 13 filters or equivalent (or higher efficiency filters) in all HVAC systems. If the system cannot function with MERV 13 filters, use the highest MERV filter grade that the system will tolerate.
(ii) Minimize recirculation of stale air. When possible, keep ventilation and furnace fans ON to bring in outside air.
(iii) Implement UV disinfection — Incorporate UV disinfection and HEPA filters into air ducts of air conditioning systems.
(iv) Institute an “open windows/doors” policy where open windows can bring in clean air — Require that windows and doors always be kept open in naturally ventilated indoor spaces, unless there is a safety, security, privacy, health, weather, or other significant reason for closing them. Note: windows should not be opened in a way that allows air to flow from COVID-19 wards to occupied outdoor walkways or into adjacent windows of non-COVID areas.
(v) Implement Local exhaust ventilation (LEV) is the application or addition of an exhaust system at or near the source of contamination (when applicable, e.g. patient ward, dentist room, etc.).
(d) HEPA purification: HEPA air purifiers should be placed in the space based upon size, layout, function and occupancy. Avoid ionizers and ozone generation that are sometimes present in HEPA purifiers.
Notes:
- Only use proven air cleaner technologies. Filter-based technologies such as portable HEPA filters, as well as ultraviolet germicidal light (UVGI), that could be used as supplementary treatment when filtration is limited, are proven to work against virus-containing aerosols. Foggers that spray chemicals into the air and electronic air cleaners (ions, plasmas, hydroxyls, photocatalysis) can be harmful and should be avoided.
- DIY air cleaners (Corsi-Rosenthal boxes with MERV-13 filters or better and fan boxes) are inexpensive air purifiers that can be readily constructed and used as an alternative to commercial HEPA filters where budgets are the limiting factor for air cleaning.
- Portable air cleaners commonly use Clean Air Delivery Rate (CADR) to describe their effectiveness. CADR is a term used to describe the amount of clean air delivered to a space as determined by filtration effectiveness and the amount of air moving through the filter. The CADR metric is valuable because it can be used to estimate the ACH of virus-free air being delivered to the room. The estimated ACH is calculated as [CADR in ft3/min × 60 min] divided by the room volume in cubic feet. A device with a CADR of 300 in a 500-square-foot room with 8-foot ceilings will therefore deliver 4.5 ACH.a. For example, if a portable air cleaner has a high-efficiency particulate air (HEPA) filter, it will capture 99.97% of aerosols at 0.3 μm. Filter efficacy is commonly reported based on the aerosol size against which the filter performs most poorly (0.3 μm), although a HEPA filter will capture an even greater percentage of aerosols larger (and smaller) than 0.3 μm.
- This same filtration concept can be applied to air that is recirculated through a central mechanical ventilation system or within-room ventilation system. Upgrading filters in mechanical systems is particularly important in buildings that use systems that recirculate air within the same room or same local ventilation zone.a. However, most central mechanical systems were not designed for HEPA filters. Instead, these systems use filters on a different rating scale, minimum efficiency reporting value, or MERV, and typically use a low-grade filter (eg, MERV 8) that captures only approximately 15% of 0.3- to 1-μm particles, 50% of 1- to 3-μm particles, and 74% of 3- to 10μm particles. For infection control, buildings should upgrade to MERV 13 filters when possible, which could capture approximately 66%, 92%, and 98%, of these sized particles, respectively.b. These MERV values can be applied to the estimate of the overall clean air delivery rate for the room as with HEPA filters, but, instead of using near 100% capture efficiency for HEPA, the calculation has to be adjusted for the lower capture efficiencies of whichever MERV filter is used.
- Engineering controls is the third of five members of the hierarchy of hazard controls, which orders control strategies by their feasibility and effectiveness. Engineering controls (like ventilation and air purification) are preferred over administrative controls because they are designed to remove the hazard at the source, before it comes in contact with the people. Well-designed engineering controls can be highly effective in protecting patients, workers, population and providing this level of protection will typically be independent of compliance of individuals to other measures.

Pillar III. Surveillance/Testing
Healthcare institutions must institute (a) Reporting of workers symptoms and testing, (b) Reporting of exposures and testing, (c) Screening of visitors through symptoms, (d) Regular screening (mass) testing of all occupants.
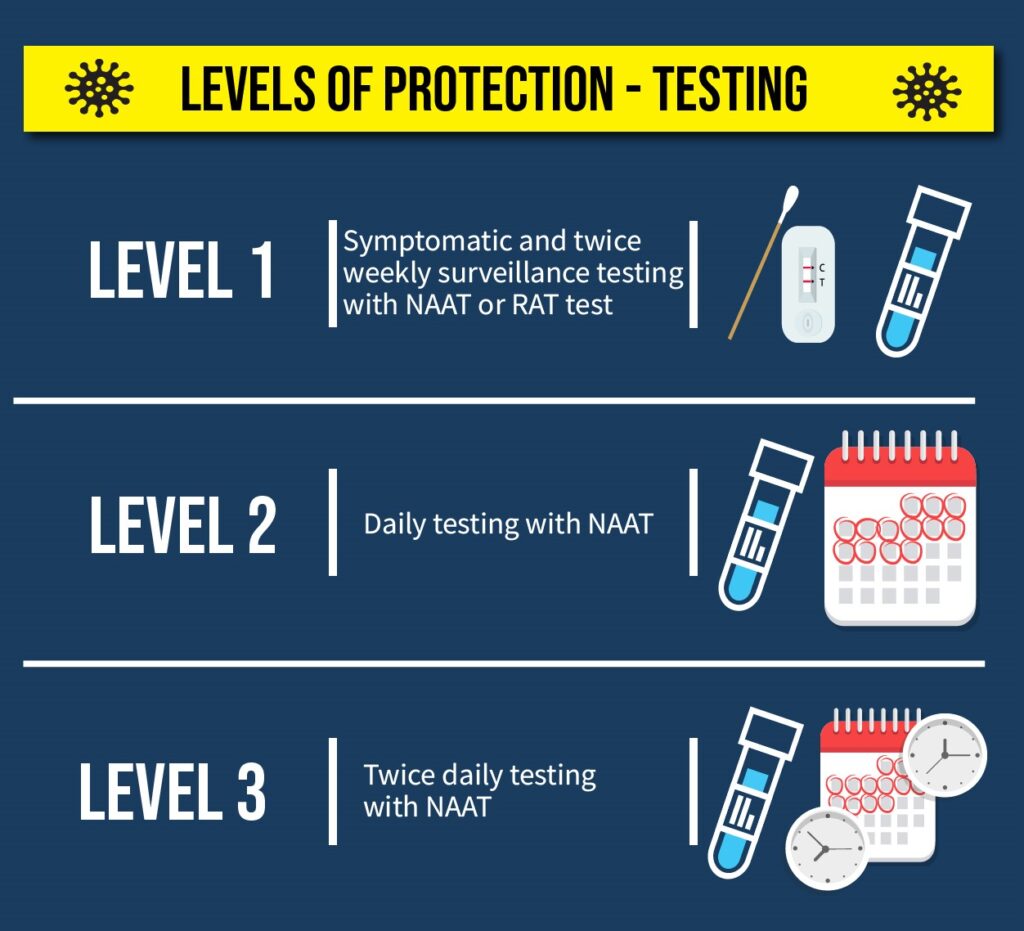
The quality of testing increases with increasing frequency of mass testing and test quality. For new variants a minimum of twice per week tests are necessary, but a better standard is daily testing, with twice daily testing (e.g. at start and end of workers shift, morning and evening for patients) serving as a way to achieve low risk for transmission. Rapid Antigen tests (RAT) may be used to identify cases, however PCR or LAMP nucleic acid amplification tests (NAAT) are significantly better, particularly for new variants.
The baseline level of protection is symptomatic and exposure (contact tracing based) testing of all individuals and twice weekly antigen or NAAT testing of all workers and resident patients.
Higher levels of surveillance are often warranted, particularly daily NAAT testing.
Higher levels of safety can be achieved by (a) increasing the frequency of surveillance testing to once daily(b) antigen tests replaced by NAAT.(c) surveillance testing of all patients and visitors.(d) increasing the frequency of surveillance testing to twice daily (e.g. at start and end of workers shift, morning and evening for patients).
Levels of action are based upon type of test and timing/frequency:
Level 1: Twice weekly testing with NAAT or RAT (less desirable due to higher false negative rates, especially with newer variants) with acceptance of positive home and outside laboratory testing results as positive without a requirement for confirmation, as well as acceptance of trusted sources of negative test results within the last 12 hours
Level 2: Daily testing with NAAT
Level 3: Twice daily testing with NAAT
For example, under conditions where standard measures for ventilation and masking are present, Level (1) Twice weekly testing should be standard for all workers interacting with other individuals whose infection status is unknown and in spaces that may have previously been occupied by other individuals over a few hours. Level (2) Daily testing should be standard when exposed to a patient with suspected or confirmed COVID-19. Level (3) Twice daily testing should be standard for workers engaging in extended time procedures requiring proximity and aerosol generating procedures.

Notes:
- LAMP tests are a low cost type of NAAT and, for surveillance purposes, have near PCR quality that can be readily implemented in house with minimal training and cost in many health care institutions.
- NAAT samples can be pooled to reduce costs by combining samples from multiple individuals, particularly from connected individuals in the same ward or office. When a test is positive, retained individual samples can be retested for each individual. This is cost effective when transmission rates are not too high.
- Where limitations on testing do not allow all workers and resident patients to be tested twice weekly, syndromic methods using thermometers and oximeters as well as sampling strategies that focus on high contact individuals and representatives of wards should be implemented.
- Screening of an entire facility is highly recommended where cases are identified outside of a COVID-19 ward. Where boundary controls between zones are implemented, full screening can be implemented within a zone, or within a zone and its neighboring zones instead of in the entire facility.
- Testing should be conducted in a manner that protects both the individual being tested and staff, whether they are asymptomatic or symptomatic. Outdoor locations for test sites is particularly recommended.
- All tests have false negative rates, so a negative test does not guarantee that an individual is not infected. This information should be provided to all individuals so that a false sense of security is avoided. At symptom onset PCR tests have a 30% false negative rate, antigen tests have an additional 30% false negative rate that has increased for recent variants including Omicron. Multiple frequent tests help to identify cases before or soon after transmission begins, which is critical to prevention of transmission and particularly larger outbreaks, especially in high contact healthcare settings.
- Contact tracing (see section on Contact tracing below) based testing includes individuals who have interacted in person with any individual who has been diagnosed with COVID-19, regardless of levels of precautions taken—unless they are consistent with precautions recommended for interactions with infected individuals, or has been in a location where an identified case was present up to several hours previously. The duration of contact does not have to exceed any threshold as being in the same physical space constitutes exposure for highly transmitting variants.
- It is essential that financial incentives are aligned with prevention so that test taking and post-testing actions are followed. This includes both management and financial support for time off, isolation, and quarantine.
Pillar IV. Social distancing and De-densify Space

To the extent possible to accomplish the work, greater distancing is better. Where possible, remote work and communications, as well as separated or partitioned indoor spaces, are better than having multiple individuals present in the same indoor space. Where it is necessary for some individuals to occupy the same space, this should not be a justification for others to do the same and by doing so increase their risk of infection. In combination with ventilation and masking, social distancing within a shared workspace reduces the risk of viral transmission by allowing aerosols to become diluted in the air between people. Social distancing should not be thought of with a strict threshold in mind (such as 6 feet); rather, the dilution of aerosols over space creates a continuum of risk. Aerosols can carry over distances far greater than 6 feet. Healthcare institutions must (a) prohibit non-essential workers gatherings and meetings, including shifting any in-person meetings to virtual if they can serve a similar objective, (b) prohibit non-essential visitors, (c) implement a variety of context specific measures to reduce in person contact and increase physical distance in the workplace.
Level 1: Maximize distance between people and de-densify spaces. In combination with high levels of protection from the other pillars (PPE, ventilation/filtration, and testing), maximizing distance between people present within a space decreases potential COVID exposure. Commonly known recommendations for spacing based on droplet-transmission assumptions (6-foot distancing) are not evidence-based and do not apply to aerosols. Distancing measures should be undertaken in conjunction with the ventilation/filtration level. Staff present within a particular space should be the minimum necessary to complete the clinical task, with exceptions made for trainees.
Level 2: Hybrid virtual/remote and in person operations. Staff needed for on-site work would be on-site only where and when needed, and would be allowed to work remotely (from home, or from a work-provided workspaces with maximized ventilation/filtration) for any activities that do not require their physical presence (such as meetings, trainings, and work other than direct clinical care or hands-on activities).
Level 3: Fully remote operations and/or separate isolated spaces for all on-site work. Where possible, clinical services transition to telehealth, and workers work remotely or from separate offices on-site.
For those having daily workplace contact with infected or vulnerable individuals, consider recommendations, requirements, or selection of workers who can limit their COVID-19 transmission exposure in non-work conditions.
The control of visitors and zoning can be considered in the context of a broader definition of social distancing. We include the discussion of these elements of prevention in this section.
Visitors and Service Providers
Discourage non-essential visitors and service providers. Note: an essential visitor is defined as necessary to the patient (or in healthcare with long term residential facilities, the resident) in terms of maintaining mental and/or physical health, or is required in specific situations including end-of-life, change in health status, other clinically indicated circumstance, or other pressing or important circumstances (e.g. financial or legal matters, family crisis). Service providers should be subject to the same conditions as visitors.
Determine clear guidelines about conditions and behaviors for which visiting is not allowed including symptoms, travel, mask-wearing, occupational risks, and so on. Inform staff, patients, and residents about these guidelines. Specific conditions depend on the healthcare settings and resident types.
Examples of visiting conditions include:
- Maximize use of remote technology. encourage and make regular practice the use of text, telephone, connectivity, digital community, and productivity platforms and videoconferencing.
- Indoor visits conditions:
- Each resident or alternate decision maker may designate one Family/Support Persons (over the age of 18) or up to two if it is essential to maintaining mental and physical health.
- Additional visitors may be given access in specific situations including end-of-life, change in health status or other pressing circumstances (e.g. financial or legal matters, family crisis).
- Outdoor visits conditions:
- Up to four individuals, including the resident, may participate in outdoor visits, with distancing requirements, if consistent with site policy and public health measures.
- Position someone at entrances to query the purpose of the visit and ask if the visitors have any symptoms, have recently traveled to areas of active transmission, or have been exposed to people with symptoms as well as proceeding with scanning temperature of the visitors. They can also provide masks if the visitor does not have their own high quality mask. Note: Entry requirements must be communicated clearly before visitors arrive at the location, only to potentially be turned away at the door.
- Provide a questionnaire for those at entrances:
- Symptoms that were present during 14 days before.
- Do they live with other people and if so ask about symptoms of household members (they may be asymptomatic but the people living with them could be symptomatic).
- Ask about travel in the last 14 days to identify the risk level of the locations of travel.
- Do they work with infected or high-risk people in their jobs (doctors, nurses, …).
- Ask them to notify if they experience symptoms within 14 days after the visit.
- It is highly advisable that people allowed entrance are tested immediately prior to entry or have been recently tested with negative results.
- Signage should be placed at entries reminding staff and visitors that an individual may be infectious while asymptomatic.
- Keep a log of all visitors with contact information and in times of higher risk call them after the visit to determine if they subsequently have symptoms.
- Visiting should be spaced at intervals to avoid crowding. Online appointments are suggested to simplify the process and reduce the risks of overcrowding the entrance pre-screening.
- Best practices guidelines should be posted in an easily readable format and relevant languages in public spaces for workers, residents and visitors to see.
- Have a designated area for visiting. Ideally, this area should have direct access to the entrance so visitors do not have to pass by various parts of the facility & should be cleaned & ventilated as often as possible (best after each visit) and having a hand sanitiser and mask station at entry. Maximize ventilation and HEPA air filtering in this area. Airborne transmission appropriate plexiglass barriers can be used to separate visitors from residents.
- Outdoor visiting is a safer option, weather permitting. These also have to be scheduled so there is not overcrowding. Tables, chairs and other outdoor equipment must be cleaned between visits.
- Spare rooms in the facility should never be used as quarantine housing for potential/positive cases.
- In times/regions of high community transmission, all visits should be prohibited except for an emergency.
- Provide for and facilitate alternate means of maintaining family contact via video calls such as- Zoom, Skype, assisted phone calls, etc., appropriate to the setting.
- Whenever possible, no-contact deliveries should be dropped off in a space that does not require entry into the facility.
- Service and deliveries that cannot be no-contact should be made by individuals who do not have symptoms of the disease and have not recently (within 14 days) had known exposures.
Zoning and Cohorting
Zoning refers to separating the physical space into disjoint areas so that protocols within each zone can be customized for the presence of infections within a zone and boundary controls can be implemented to prevent transmission from zone to zone, enabling reduced level protocols within zones that have inherently lower risks.
An essential use of zoning is the distinction between COVID-19 wards and non-COVID wards. Higher levels of precaution in COVID-19 wards can be more clearly specified and more easily implemented due to reduced uncertainty about which protocols to follow. Boundary controls serve to prevent contagion between COVID-19 and non-COVID wards. Boundary controls include restriction of individuals going between wards, as well as disinfection protocols at boundaries between wards.
Cohorting generally refers to the grouping of patients with the same condition, along with the staff caring for those patients, in a defined area (that is, within a room, section or building) to minimize risks. Cohorting of staff can be considered a component of zone boundary control.
Risks increase if workers from non-COVID wards share a space / air with someone who is a confirmed case or with staff who are caring for confirmed cases. Boundary controls should include measures to prevent in-person meetings or shared dining of workers from different zones.
For effective boundary control it is essential to have a good understanding of the air handling systems, source of air, flow of air, and recirculation in a healthcare facility including hallways outside and between zones. Measures for mitigation of risk include implementing additional air filtration at boundaries, and/or creating buffer areas that are considered part of the zone boundary.
The use of zoning and cohorting should not be limited to the distinction between COVID-19 and non-COVID wards. In particular, distinguishing multiple non-COVID wards and imposing boundary controls and cohorting provides an important method of prevention of larger outbreaks. If transmission occurs to/in a non-COVID ward, the resulting outbreak is likely to be contained before it is recognized, and larger outbreaks prevented. Green zonePatients and staff with no COVID-19 risk factors. Previously confirmed COVID-19 patients who are after recovery and are cleared as being no longer infectious may be located in a Green zone.Yellow zoneClose contacts in quarantine or patients who are in preventive isolation.Red zoneSuspected or Confirmed COVID-19 cases that have not met department clearance criteria. This may be one or several patients (for example, on a ward).
Note on nursing homes and other residential high risk institutions:
It is essential that nursing homes and other High-Risk institutions that do not inherently serve infected individuals follow “Safe Zone” practices and remain disease-free. When COVID-19 is found in a nursing home, the confirmed case and suspected cases (if any) should be immediately isolated from others and from each other (confirmed from suspected cases, and multiple suspected cases must be isolated from each other in case one of them is infected and the others are not, multiple confirmed cases may be isolated together). Off-site isolation should be facilitated when possible. Health care workers and individuals who are not yet known to be infected should wear proper PPE throughout the facility until it can be determined that the outbreak is confined to isolation areas. Unnecessary personnel should be forbidden in isolation areas. Strict disinfection should be carried out for isolation areas and contaminated objects (see also Appendix B).
Pillar V. Vaccination
Vaccination is a key measure to reduce the risk of developing severe acute COVID-19 infection (including hospitalization and death) for individuals who are vaccinated; however, people who are up-to-date with COVID-19 vaccinations can easily become infected and transmit the virus to others. Therefore, it is not as effective as the first four pillars described above in reducing transmission risk in a health care setting for workers or patients. People who are up-to-date with COVID-19 vaccinations can still develop symptomatic infection, requiring time off work to recover. People who are up-to-date can also develop long COVID, which may lead to development of long term chronic illness and disability.
Thus, vaccination requirements do not reduce or eliminate the need for a robust layered approach to prevent transmission of COVID-19 in the workplace. Vaccination should be deployed as part of a “vaccines-plus” strategy in the fight against COVID-19. This strategy utilizes a combination of vaccination, public health measures, and specifically the five pillars that are outlined in this document.
It is important to note that COVID-19 infection does not provide lasting immunity and should not be considered as an alternative to vaccination or other preventative measures.
SECTION C: Measures Supporting the Five Pillars
Supporting Measure 1. Contact Tracing
In keeping with known airborne transmission of COVID-19, contact tracing must be implemented under the assumption that individuals working together within an indoor space without fully isolated ventilation with an identified COVID-19 case (index case) should be considered potentially exposed, regardless of the levels of protection in place, unless the implemented measures are consistent with treatment of a known infected patient. Also, aerosols may persist in the air for hours; thus, individuals who entered a room for several hours after an index case left would also be considered exposed. Time and distance could be included in prioritization of case investigation but should not be used to limit the extent of contact tracing, as under previous droplet-transmission criteria (e.g. 6-feet distance and less than 15 minutes are insufficient safety criteria according to available data).
Notification systems including both work e-mail and other channels (e.g. text or smart phone notifications) should be utilized to ensure that exposed individuals can isolate appropriately from household members and other contacts, particularly those who may be at a high risk of severe COVID-19. Measures should be undertaken to protect the privacy of the index case; however, these measures must not impede timely notification of exposed individuals. Delays in notification and quarantine/testing of exposed contacts have the potential to lead to larger outbreaks.
It is the responsibility of employers to ensure that adequate contact tracing occurs for workplace exposures. In areas where local public health offices do not provide sufficient contact tracing services, employers should train workers to conduct contact tracing within the organization. In addition to reporting cases to local public health authorities, employers should consider making aggregate case data available publicly (e.g., through a public dashboard website).
Contact tracing should also include visitors and outside providers. Healthcare institutions should ask visitors and outside providers to report infections up to two weeks after a visit to the facility, and close contacts up to two weeks prior to a visit who report infections from then until two weeks later. A log of all visitors with contact information should be compiled and they should be called after the visit to determine if they subsequently have symptoms. They should also be informed if there were potential exposures at the healthcare facility.
Supporting Measure 2. Quarantine and Isolation
Robust quarantine and isolation policies, with appropriate financial and administrative support, can prevent viral transmission, reduce the size of outbreaks, as well as ensure that COVID-19 positive workers have adequate time to rest and recover. The current 5-day quarantine / isolation is insufficient, even when combined with testing, and is likely to lead to significant workplace outbreaks due to ongoing infectiousness. In addition, returning to work prematurely during an active infection can increase both the difficulty of recovery and long term harm to workers. A 14-day quarantine/isolation period is the recommendation, as outlined below (see also guidelines on Isolation). Quarantine is the terminology used for individuals who may have been exposed to COVID-19, while isolation is the terminology for individuals who have tested positive for COVID-19, with or without symptoms.
Implementation of a 14 day isolation/quarantine period has been seen as a burden due to the duration of absence of an individual worker from a facility. However, the prevention of transmission will reduce both the number and frequency of worker absences, and the magnitude and duration of workplace outbreaks.
Quarantine should be implemented when indicated by contact tracing (see Section C, item 1), when lapses in mitigations occur in caring for known or suspected COVID-19 patients, or when workers develop new symptoms. The recommended minimum length of quarantine is 14 days, with two sequential negative NAAT separated by 24 hours required to exit quarantine. Testing during and at the end of quarantine provides identification of asymptomatic cases, and earlier identification of presymptomatic cases. This early identification allows workers to better assess risk to their household members and to seek medical care including treatment earlier. For workers in quarantine who are asymptomatic, remote work options or paid time off should be made available as appropriate to the job role, skills of the individual, and needs of the organization. Individuals who become symptomatic or test positive during quarantine should begin isolation from that time.
For workers who test positive for COVID-19, 14 days is the recommended minimum isolation time period, and longer isolation may be needed in order to allow for resolution of symptoms or two negative NAAT separated by 24 hours. Symptoms associated with the illness should be completely resolved for 3 days prior to exit from isolation. Consider that COVID-19 may present with a variety of symptoms, which are not limited to the respiratory tract. Two negative NAAT tests separated by 24 hours are required to exit isolation. Paid time off is preferred rather than remote work for the duration of the isolation period, as rest is needed in recovery from COVID-19 and prevention of Long COVID.
We note that there is limited scientific support for reducing the infection isolation period to 12 or 10 days. However, this should be done with additional precautions, including avoiding in-person meetings, after exiting isolation. Similarly, where NAAT exit testing is replaced by RAT testing, additional precautions should be taken for several days after exiting isolation due to possible false negative tests, which occur at a higher rate for Omicron and later variants.
Return to work for individuals who have tested positive for COVID-19 should include a fitness-for-duty evaluation and reduced/modified work duties during the recovery period. Many individuals experience a variety of symptoms during recovery or develop post-COVID sequelae known as Long COVID (current estimates are conservatively 10-30% of individuals who are infected), and additional physical and mental health support is recommended during an extended period following infection.


Supporting Measure 3. Hygiene
Surface hygiene is secondary to air cleaning for COVID-19 but the widespread contamination of surfaces has been documented and transmission from them continues to be a concern. Frequent cleaning of high contact areas and general disinfection continues to be an essential precautionary measure. Measures to be implemented:
- Reduce touch points, by implementing, e.g. motion sensor light switches, automatic door opening, IR sensitive toilet flushing, automatic soap dispensers (note that air blower hand dryers are known to increase aerosolization in rest rooms and should be avoided).
- Clean and sanitize high-frequency touchpoints at a pace compatible with the usage. These include door handles, elevator buttons, sinks, toilets, tabletops and frequently handled machinery, equipment, electronic devices and other items. Particular attention must be devoted to hand grips and stair rails.
- Check and ensure that soap dispensers and paper towels in bathrooms remain adequately supplied throughout the day.
- Provide hand sanitizers at all entrances, exits and high-traffic locations.
- Provide tissues and sterilizing alcohol-based wipes.
- Replace commercial-style open-ring dropdown toilet seats with those fully covering, and post signage encouraging closing before flushing (may reduce aerosolization from toilets, this mechanism of fecal to airborne transmission has been confirmed).
- Install electronic (IR) switches, or elbow-operated faucet handles or foot-operated sink controls to minimize need for hand surface contact following hand-washing. Provide signage instructing in use.
- Engineer door-opening and closing to minimize need for hand surface contact following hand-washing or use of restroom, or for the entrance to the buildings, or when crossing different sections of a building.
- Where hand surface contact is needed to open doors on entry or exit from restrooms, place disposable towels/tissues and waste containers so they can be used for contact.
- Use paper towels for hand drying. DO NOT use air blower hand dryers as they are known to widely spread viral particles.
- Cell phones (personal or work-issued) being used by workers can be a source of contamination. Cell phones should be disinfected regularly or carried in a plastic sealed bag that can be decontaminated, especially when moving between different zones. Hand hygiene should be performed before and after cell phone use.
- Other high-touch equipment such as computer keyboards, touch screens, tablets, and other human interface devices should be regularly disinfected, and hand hygiene should be performed before and after use.
Supporting Measure 4. Conditions for attention
Dining rooms
- Shared dining facilities are high risk areas for transmission.
- A shift to individual dining or dining grouped by household should be made where possible.
- Individuals should mask when not eating or drinking.
- Level 2 ventilation measures, including elevated levels of ventilation and HEPA purification are necessary.
- Lower density dining should be implemented by use of outdoor or additional indoor food service spaces for dining, expanding their hours, as well as regulating densities.
- Occupancy of dining facilities includes patients and visitors and their use of the central dining facilities should be limited where it is not essential.
- Level 3 ventilation measures including analysis of airflows for the placement of HEPA purifiers, are highly recommended, and are necessary where high density occupancy cannot be avoided.
- Wait and service staff should avoid contact and proximity and wear elevated level masks (Level 2: elastomeric masks) and other PPEs.
- In residential facilities such as nursing homes, where residents are sufficiently autonomous, provide in-room food service with no-contact prepared food delivery.
- Sanitize high contact areas after each individual use, including tabletop, chair armrest, menu. Use washable or disposable tablecloths and menus.
- Give support and tools (hand sanitizers or access to sink, soap, and water) for hand hygiene before eating.
- Where organized dining occurs, stagger dining times to avoid crowding and sitting arrangements to avoid face-to-face dining.
- Where contact is essential for services provided, careful handling protocols should be made including effective ventilation, higher level PPEs, gloves, and disposable gowns.
- The high risks posed by dining indoors should be communicated with workers so that they prioritize other options (e.g. eating outdoors or in their cars).
Break rooms
- Break rooms are often used for dining, changing, lactation, and may have associated bathroom facilities. High levels of precaution are needed in order for those activities to be safe. * Since masks may be removed and current occupancy is not an indication of recent occupancy, careful signage and guidance is essential.
- Requirements for break rooms should include elevated levels of ventilation and air filtering (at least Level 2) and masking when not eating.
Bathrooms
- Bathrooms are areas of high risk for transmission both due to high density of use and the aerosolization of fecal particles.
- Level 2 ventilation measures, including elevated levels of ventilation and HEPA purification are necessary.
- Level 3 ventilation measures including analysis of airflows for the placement of HEPA purifiers, e.g. in each stall, are highly recommended.
- Encourage individuals to continue masking while in the bathroom.
Safe spaces for donning and doffing PPE
- PPE may need to be removed or changed throughout the course of a day.
- Safe spaces should be created where respirators can be removed in order to change or adjust them. Due to the nature of this activity, high level air cleaning and limited or sole occupancy social distancing measures will need to be implemented in this space.
- Laundry for employer-provided uniforms (scrubs) should be provided.
Medical laboratory
- Medical laboratory environments are generally restricted from patient access. However, special COVID precautions are essential due to the nature of working conditions.
- Where there is a need for in-person collaboration and troubleshooting at benches and microscopes, social distancing may not be possible to the extent it may be achieved in other areas. Thus, enhancement of the other pillars is required.
- Processing and testing of patient samples may create a risk of producing aerosols (e.g. pipetting and centrifugation). Generally, as a precautionary measure, the risk of aerosol exposure should be limited by enhanced laboratory procedures (e.g., pipetting technique, use of biosafety level 2 cabinets, increased PPE levels, etc).
- Use of remote technology including video conferencing and remote microscopy approaches (telepathology, digital pathology, and whole slide imaging) should be encouraged to facilitate social distancing, training, and collaboration.
Office workers
- Office workers that are not workers but work in healthcare facilities, and workers with offices in healthcare facilities, should follow prevention guidelines that are appropriate to office work in general, including where possible:
- work remotely
- avoid in-person meetings
- use virtual communications
- enable offices and conference rooms that are not being used to serve for individual dining for others, with appropriate enhancement of air quality (Levels 2 or 3) and cleaning before and after use.
- Where office workers must work in the healthcare facilities, they must:
- avoid all patient care areas
- participate in training appropriate to COVID-19 protection in areas they may commonly enter
- follow PPE requirements in areas that they must pass through, and in their offices if they are not alone
- use individual offices for their own dining
- Office ventilation and air filtering requirements should be established based upon usage of those offices.
- Where offices have more than one individual regularly present, high levels of ventilation and air filtering are necessary (Level 2 or Level 3) as well as masking at least at Level 1.
Other non-patient care workers and work areas
- Workers who are not workers but work in healthcare facilities should follow prevention guidelines that are appropriate to their role and work.
- Where these workers enter patient care and other areas within the facility, they should follow PPE requirements in those areas and complete training as appropriate to their role.
Supporting Measure 5. Special Accomodations
Contact with infected individuals is common for those who are caring for them. The high probability of infection in a healthcare setting means that workers have a greater chance of infection compared to community members. Despite high levels of precaution, the risk of workers infecting their own families, housemates, and others through out-of-work contact must be recognized. Whether for a new zoonotic virus, new variants, or inadequate specific data, the risks in the healthcare setting may not be adequately understood to establish guidelines that will prevent all transmission. Given the exposure risk, workers may need to quarantine frequently (see Section C, item 2: Quarantine and Isolation). The nature of contact that does occur must be carefully evaluated for determination of when quarantine is needed. Under some conditions, it is advisable to consider ongoing quarantine housing for workers to protect household members and the community. For other workers, special accommodations may be needed when they must be protected from community transmission due to the care they provide to vulnerable uninfected individuals, as in a nursing home.
Supporting Measure 6. Institutional processes
Responsibility
- Designate an Infection Prevention and Control Officer with adequate time and resources to support implementation of the institutional COVID-19 plan. This is akin to the requirement for Safety Officer in biological/chemical research labs.
- Designate leadership/decision-making authority chain allowing for after-hours and disruptive events such as short-notice need for isolating multiple residents.
- Increase emphasis on / allocation of resources for ongoing short-format staff training – “in-services,” to stay current with evolving best practices for all staff.
- Institute proactive contingency planning for positive COVID notifications, and for the possibility of a superspreader event, causing staff outages.
- Communicate with US HHS HealthCare Coalition Preparedness representatives or national equivalent.
Organizational considerations
- Prepare for employee substitutions in case they become ill individually or collectively. Where possible, cross-training in related areas is recommended.
- Implement proactive staff shortage contingency planning, including use of additional temporary or redeployed trained staff.
- Stay abreast of current public health information and advisories, and communicate updates of importance to staff on a regular basis.
- Replace in-person office meetings with virtual ones.
- Implement staff buddy-care or other programs as appropriate to monitor for fatigue and burnout.
- Put in place redundant/resilient staff emergency contact procedures.
- Provide guidance for outside providers of services and for minimizing staff and patient contact with outside providers.
Record Keeping
- Set up a reporting system for any cases.
- Keep a secure log of all visitors with contact information.
- Request all symptoms and keep a record of them for workers, visitors and outside providers.
- Request all symptoms of housemates and other close contacts.
- Request all travel information for workers, visitors and outside providers, including cities to which they travel to find out if they are more at risk of contagion.
- Record case lists – tabular record of workers, other staff, visitors and outside providers, with potential COVID symptoms and positive test results.
- Integrate all case lists with patient records, or export selected patient information into records that include workers, other staff, visitors and outside providers.
- Track and identify trends in weekly totals of acute care transitions – upticks have shown to be an early independent indicator of a possible outbreak.
- Participate in national reporting, e.g. US Centers for Disease Control and Prevention National Healthcare Safety Network – Long-term Care Facility Module (CDC NHSN LTCF) or other nation equivalent.
Education, Training, and Signage
- Implementation of these guidelines will require education to address erroneous assumptions and misunderstandings due to the existing misinformation in widespread public communications.
- Educate staff and their families, as well as patients and visitors, about COVID-19 transmission and prevention, with an emphasis on airborne transmission.
- Training should include information about how workers’ COVID-19 exposure outside of work can put coworkers and patients at risk and should include ways to get support in reducing COVID-19 risk at home.
- Training should, at a level appropriate to each employee, emphasize the scientific basis behind the precautions being taken and the importance of these precautions to protect workers, patients, and visitors.
- Training should utilize effective age-appropriate (child or adult) learning approaches and be offered in multiple formats to be accessible to staff across roles, shifts, and settings within the institution. Virtual formats should be used when possible.
- Provide effective and simple signage throughout the facilities both providing basic information and identifying specific requirements for locations.
- Ensure workers know that when they have even mild symptoms they should not be at work locations or in-person meetings, and they will be paid and not penalized for sick days.
- Ensure workers have appropriate health insurance policies so that they will not be afraid to seek out care when they have symptoms, even mild ones.
- Ensure a proper and continuous supply of PPE for the workforce.
- Document proactive contingency plans for temporary PPE supply-chain interruptions.
- Consider making masks available for employee families and household members as well as patient and visitor families.
SECTION D: Accountability for Protective Measures
Regulatory agencies and institutions should establish fines or penalties on organizations that fail to implement COVID-19 measures. Following significant outbreaks among individuals who shared the same indoor space, an audit should be conducted of policies and their implementation including for masking, air quality, testing and social distancing and supportive measures. Systemic interventions should also be considered including:
- Strengthen accountability through the creation of an internal and/or external comprehensive review body;
- Increase transparency and accountability for the institutional commitment to avoiding repeating failure to protect staff, patients and other individuals; and,
- Enhance oversight through the appointment of a Commissioner or of an independent officer with similar responsibility and capacity towards the organization.
APPENDICES
APPENDIX A: Hierarchy of Controls
Mitigation strategies that have been addressed fall into the well accepted strategies of PPE, administrative controls, and engineers controls. They include the following:
- PPE
- Respiratory Protection – Masking
- Gloves
- Eye protection
- Protective gowns
- Administrative controls
- Surveillance and Testing
- Social distancing and occupancy density
- Isolation and quarantine procedures
- Vaccination
- Hygiene
- Boundaries: visitors
- Record keeping
- Education and training
- Engineering controls in spaces (healthy building and work environments)
- Ventilation and air purification via HEPA filtration
- CO2 monitoring
- Local exhaust ventilation (LEV)
APPENDIX B: Nursing Homes and Other High Risk Facilities
Employees, facilities, and work environment
- Emphasize to workers that their actions outside of work can lead to transmission within the healthcare setting. Education should include how to mitigate risk to their families and households as well as to residents of the facilities where they work. Even if the disease has a low risk to them, any contact with individuals or surfaces in non-safe areas is extremely dangerous for those in the high-risk facility. They should take responsibility and limit off-work non-safe contact to a minimum, while their employers/facilities are making face coverings and/or masks available to their close relatives.
- Encourage workers’ adoption of safe space protocols at home limiting their contact and others who live with them with individuals and surfaces that are not safe and record which workers are following them on a voluntary basis. Note: a “Safe space” is defined by the CDC as a space where people can self-isolate or practice social (physical) distancing between themselves and other people who are not from the household.
- Employers should adopt and communicate with workers and supervisors in order to prioritize and plan as soon as possible to: ○ pay workers enough so they don’t need multiple jobs to subsist. ○ give workers enough hours so that they can work in only one place, and get good health insurance for themselves and their families. ○ find appropriate staffing levels for each type of worker so that there are the minimum number of staff coming in and out, and at the same time preventing overwork, exhaustion, burn out.
- Ensure additional and greater supplies of PPE equipment for the workforce. As a supplementary measure, ensure masks are available for workers’ families.
- Engage with local medical facilities/laboratories or local and state/provincial public health agencies, to coordinate rapid testing and contact tracing of residents and workers.
- Partition facilities to separate zones, limiting workers and residents from crossing from one zone to another. This will limit contagion, in case one zone becomes infected.
- Stagger breaks and discourage socializing within indoor confined areas. Ensure mask wearing even for staff-staff interactions and ensure proper training in PPE wearing/fitting.
- Transfers of residents in or out of the institution should follow safe space requirements with attention to point of origin, point of destination, contact with those performing the transfer, and the vehicles that are involved.
- When bringing in new residents or starting new workers who are not coming from a Safe Zone quarantine for 14-21 days.
- Where possible, arrange facilities for residential accommodation of workers within this or another Safe Zone.
- Arrange partnerships with sister institutions to follow Safe Zone practices for transfers and response to an outbreak.
- Arrange for office staff to work from home, develop protocols so that this is possible.
- Avoid clustering in elevators. Elevators should not take more than half of their carrying capacity.
- When AC is used, disable re-circulation of internal air. Clean/disinfect/replace key components and filters weekly.
- Check the engineering design of the ventilation system to determine if air flows connect air from different rooms. Develop mitigation or alternative ventilation processes.
- Deploy HEPA air purifiers around the facility.

